Mental health literacy refers to the knowledge and beliefs that help individuals recognize, cope with, or prevent mental illness (Jorm et al., 1997). Cultivating individual mental health literacy helps with the early identification of mental health issues as well as appropriate intervention, preventing mental health decline, reducing the stigma associated with mental illness, and reducing delays in seeking treatment (Jorm, 2012). Healthy China Action (2019–2030) has set the goal of widespread improvement in the mental health literacy of the general Chinese population by 2030, emphasizing that “enhancing mental health literacy is one of the most fundamental, cost-effective, and efficient measures to improve mental health.” Scholars have conducted extensive research on the mental health literacy of college students both prior to and during pandemics, including their mental status (Roberts et al., 2011), assessment (Tambling et al., 2023), and interventions (Beasley et al., 2020; Reichel et al., 2023; Reis et al., 2022). The significant amount of research in this area reflects to some extent the high prevalence of mental health issues among college students in the context of the COVID-19 pandemic (Hu et al., 2021). However, the potential ability of mental health literacy to reduce mental illness and psychiatric consequences remains unexplored.
In the face of sudden public health events, an individual’s mental health literacy is an important factor affecting their physical and mental health. Numerous empirical studies have indicated that sudden public health events may first impact individual health and subsequently affect the mental health of groups (Roberts et al., 2011). Cai et al. (2021) found a significant improvement in the mental health literacy of those aged 15–59 years in China, suggesting that during the COVID-19 pandemic, individuals may have acquired more health knowledge, identified psychological assistance needs, and investigated accessible resources and assistance to improve their mental health. From a positive psychology perspective, personal experience or witnessing traumatic events may lead to negative mental reactions such as posttraumatic stress disorder, depression, and anxiety; however, it may also lead to positive changes to the mental state, which is known as posttraumatic growth (Tedeschi & Calhoun, 2004). Examples of posttraumatic growth in a sudden public health event include learning how to overcome adversity, changing awareness and behavior, and achieving self-transcendence in response to environmental changes. Although these studies provide an important contextual overview of the causes and effects of sudden public health events, little research has compared changes in mental health literacy before and during an outbreak. In addition, previous research has focused on either the negative or the positive impacts of pandemics on mental health, rather than holistically examining both types of impact together. To fill this research gap, this study used the mental health literacy of college students in 2019 as baseline data, comparing their literacy levels with data from 2022 to examine changes occurring after the outbreak of COVID-19.
Method
Participants and Procedure
We used convenience and snowball sampling methods to survey 2,249 college students before the COVID-19 pandemic (May–June 2019) and 3,007 college students during the COVID-19 pandemic (May–June 2022). Before filling out the survey on the Wengjuanxing online platform, participants were required to provide informed consent. They completed the survey on a voluntary basis in approximately 10–15 minutes, then had the opportunity to receive a randomly distributed cash reward through a raffle. The Academic Ethics Committee of Huzhou University approved this study. We eliminated 52 and 131 invalid questionnaires that contained obvious unqualified logic, too-short an answering time, or failed the attention-check items, resulting in 2,197 and 2,876 valid questionnaires (recovery rates of 97.69% and 95.64%, respectively). Participants’ age ranged between 16 and 26 years in 2019 (M = 19.81, SD = 1.65) and between 15 and 26 in 2022 (M = 19.77, SD = 1.90).
Measures
Demographic Variables
We collected participants’ demographic information, encompassing individual factors (age and gender), school roles, and family residential region. Within the age category the response options were ≤ 17 years, 18–19 years, 20–21 years, 22–23 years, and ≥ 24 years. In the gender category the options were man, woman, and transgender. In the school roles category the options were general students, referring to students who did not hold any positions; psychological commissars, comprising the students who looked after their classmates’ mental health, which is a unique student role found in universities in China; psychological department student cadres, referring to those from the psychological department within the student union of their school or college; and other student cadres, comprising student cadres from other departments of the school or college. Regarding family residential region, the options were eastern, central, western, and overseas. Table 3 contains the details regarding these demographic variables.
Mental Health Literacy
We employed the 75-item National Mental Health Literacy Questionnaire (Ming & Chen, 2020), which includes three subscales: mental health knowledge, mental health behavior, and mental health awareness. The mental health knowledge subscale has eight dimensions comprising 50 true/false items covering various topics, including the causes and prevention of mental illness, symptoms and recognition of mental problems, treatment of mental disorders, psychosomatic health, crisis intervention and suicide prevention, child education, child protection, and other fundamental knowledge and principles. The score range for this subscale is 0–50, with each answer scoring either 0 points or 1 point; higher scores indicate a greater level of mental health knowledge.
The 16-item mental health behavior subscale includes four dimensions covering emotional identification, cognitive reappraisal, interpersonal support, and distraction/attention shifting. Items are rated on a 4-point Likert scale ranging from 1 (never) to 4 (always), with higher scores indicating healthier behavior.
We used the nine-item mental health awareness subscale to evaluate the importance of mental health. Items are rated on a 4-point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree), with higher scores indicating a greater emphasis on mental health.
Respondents’ mental health literacy score is calculated as the sum of their scores for mental health knowledge, mental health behavior, and mental health awareness. Cronbach’s alpha was .77 in this study and the Kaiser–Meyer–Olkin value was .91 (p < .001), demonstrating good reliability and validity.
Results
College Students’ Mental Health Literacy Scores Before and During the COVID-19 Pandemic
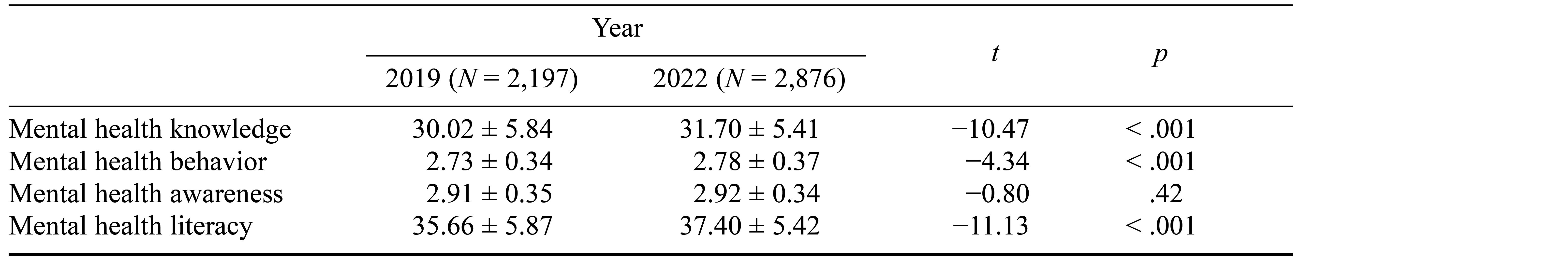
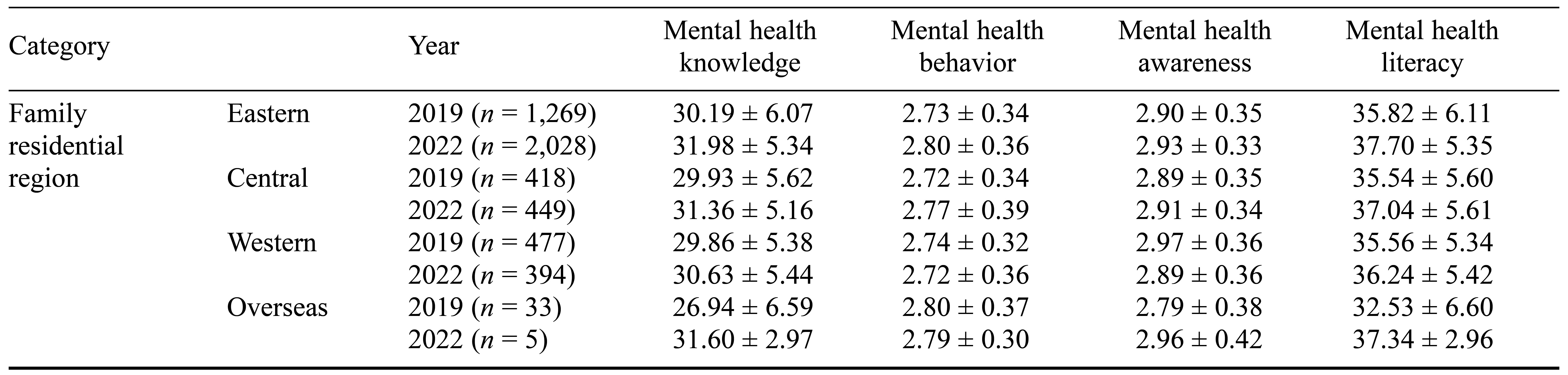
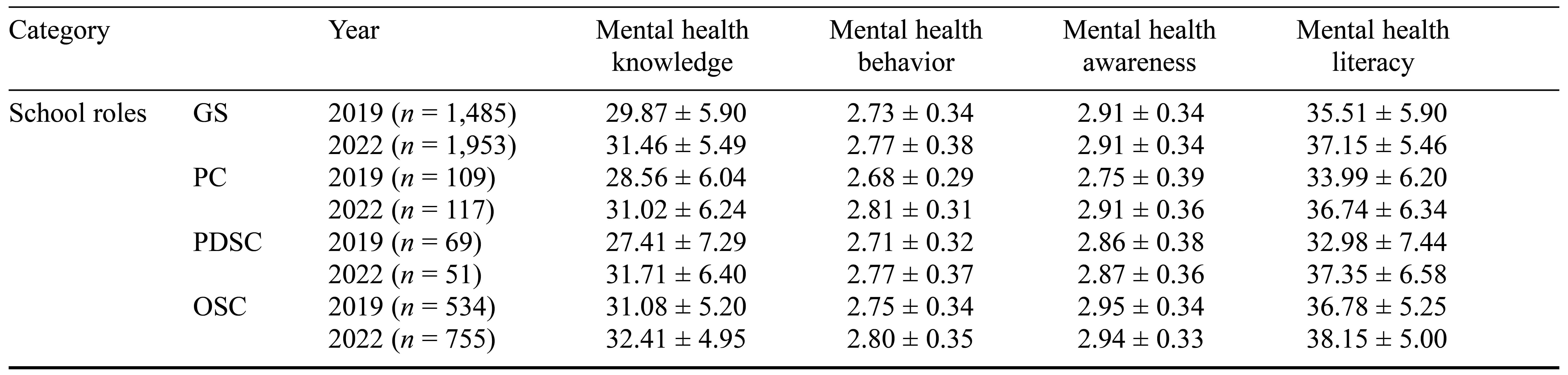
We conducted independent-sample t tests to compare students’ mental health literacy scores before and during the COVID-19 pandemic. The results indicate that mental health knowledge, mental health behavior, and mental health literacy were significantly higher during the COVID-19 pandemic than before the pandemic (p < .001; see Table 1).
Table 1. Comparison of College Students’ Mental Health Literacy and Various Dimensions Before and During the COVID-19 Pandemic
Category Analysis of College Students’ Mental Health Literacy Before and During the COVID-19 Pandemic
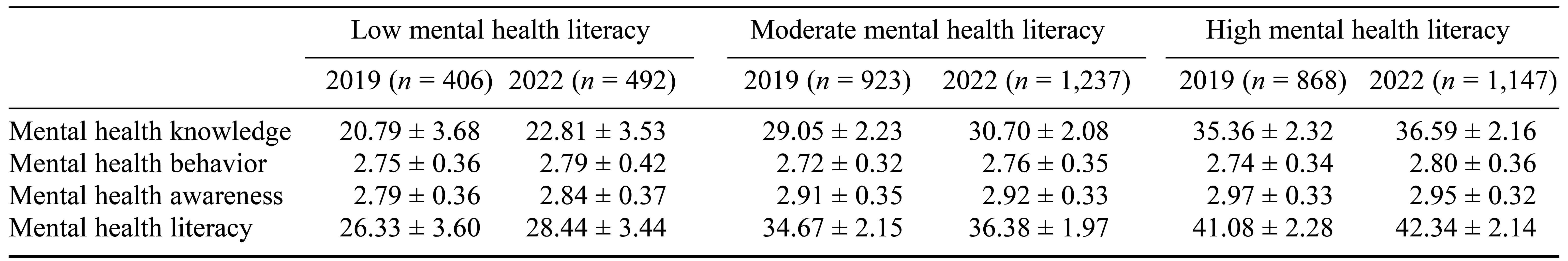
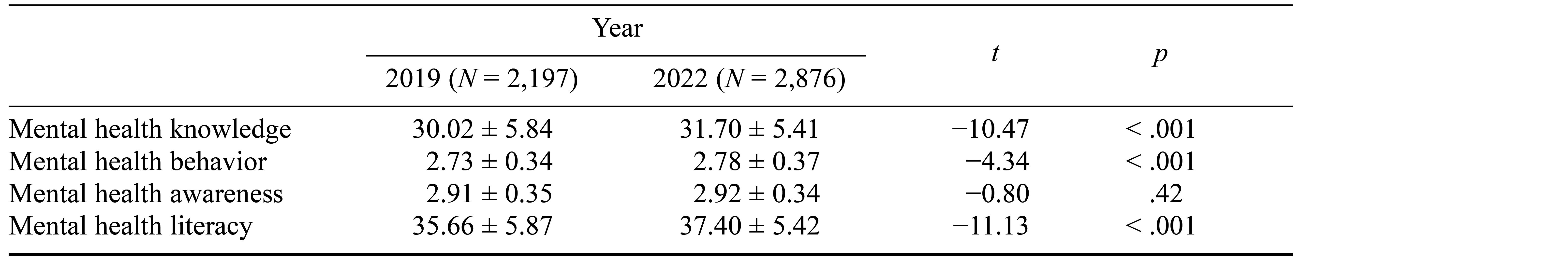
We employed cluster analysis of the data using the K-mean Q method, categorizing the participants into three groups: high mental health literacy, moderate mental health literacy, and low mental health literacy. In 2019, the proportions of these three groups among the college students surveyed were 39.51%, 42.01%, and 18.48%, respectively. In 2022, the proportions of these three groups had shifted to 39.88%, 43.01%, and 17.11%, respectively. We further examined the differences among these groups across our three measured dimensions of mental health literacy (knowledge, behaviors, and awareness). There were significant differences across all three dimensions, χ2mental health knowledge = 2.66, χ2mental health behavior = 4.30, χ2mental health awareness = 9.05, p < .05; Fmental health awareness = 40.63, p < .001 (see Table 2). Thus, there were more students with high and moderate mental health literacy during the COVID-19 pandemic, while there were fewer students with low mental health literacy.
Table 2. Mental Health Literacy Scores of College Students Before and During the COVID-19 Pandemic
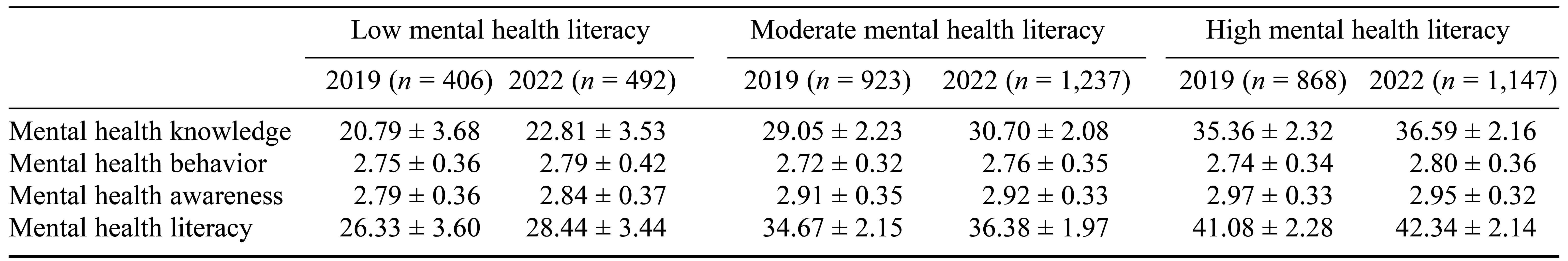
Note. Scores are mean ± standard deviation.
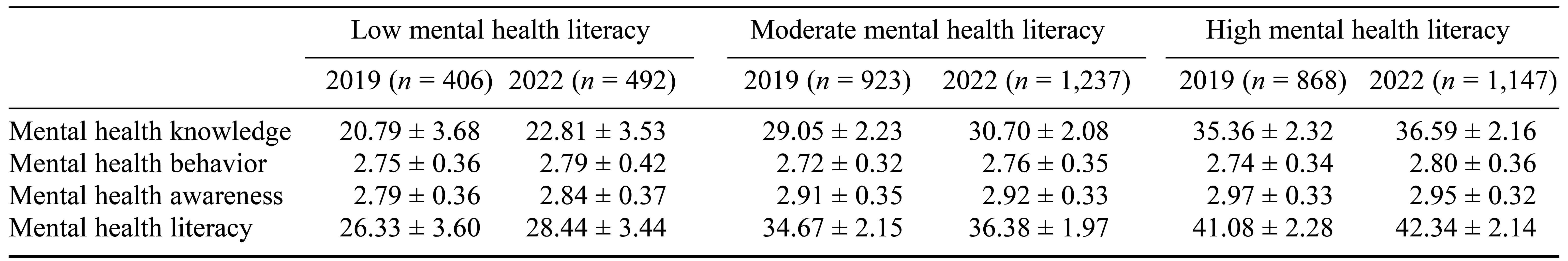
Analysis of Different Impact of Individual Factors on College Students’ Mental Health Literacy Before and During the COVID-19 Pandemic
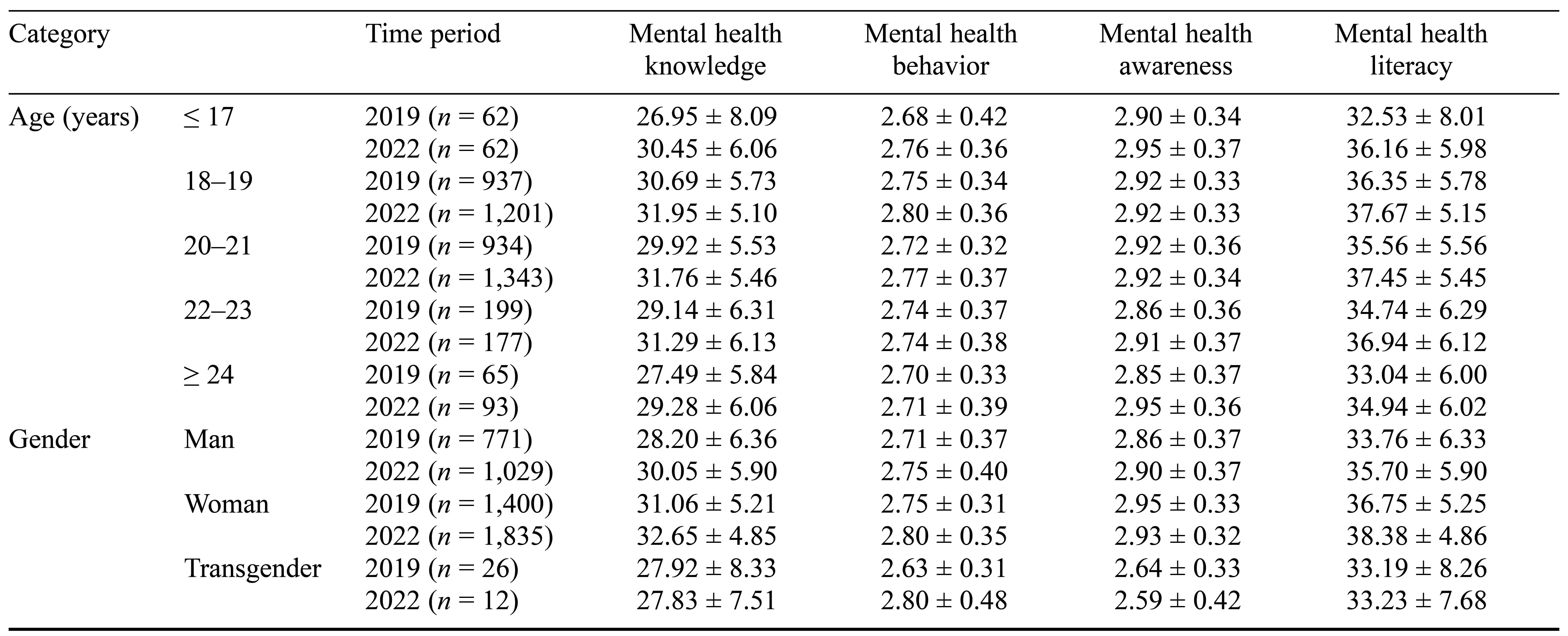
To explore the different impact of individual factors such as age and gender on the mental health literacy of college students before and during the COVID-19 pandemic, we conducted a two-way analysis of variance (ANOVA) investigating the interaction terms of age and time period, and of gender and time period. The interaction of age and time period had a nonsignificant effect on mental health knowledge, mental health behavior, mental health awareness, and mental health literacy. Only the interaction term of gender and time period had a significant effect on mental health awareness, F(1, 4) = 5.21, p = .005. A simple effects analysis showed that in terms of gender, only men’s mental health awareness during the COVID-19 pandemic was higher than before the pandemic, F = 8.68, p = .003 (see Table 3).
Table 3. Comparison of the Impact of Individual Factors on College Students’ Mental Health Literacy Before and During the COVID-19 Pandemic
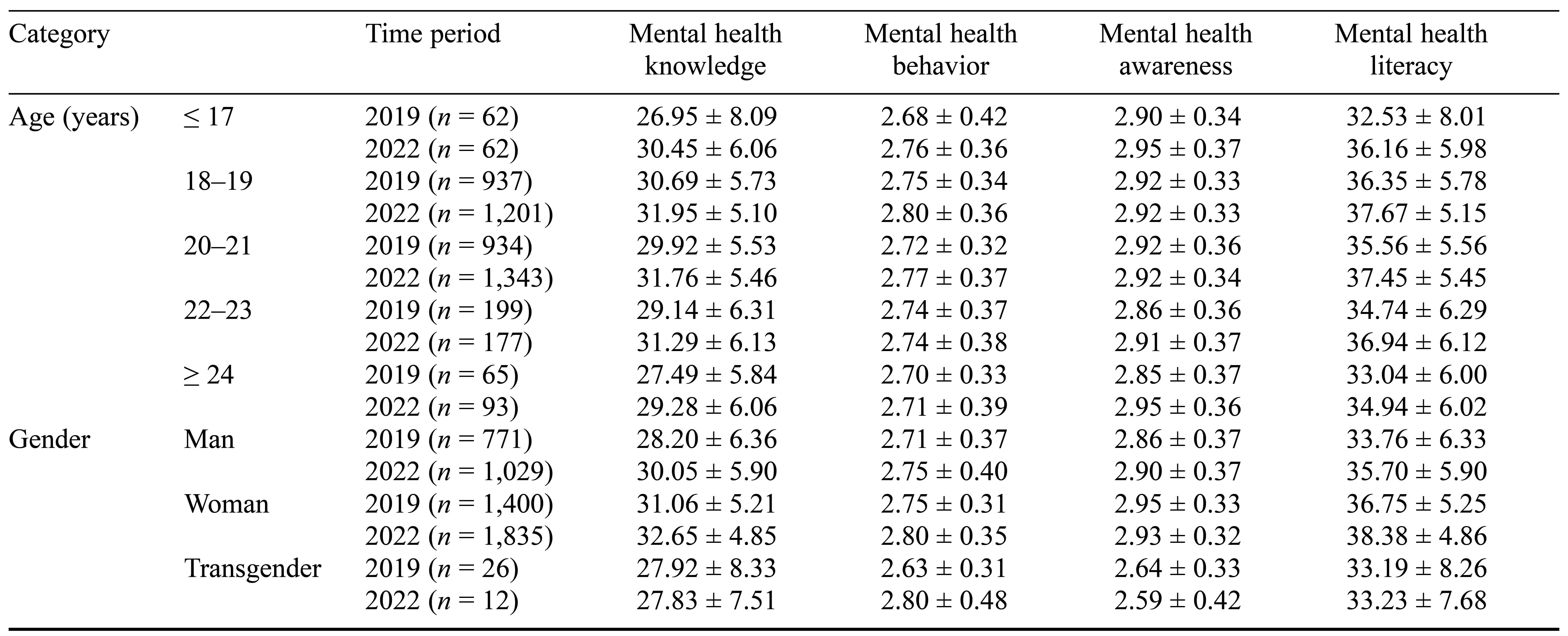
Note. Scores are mean ± standard deviation.
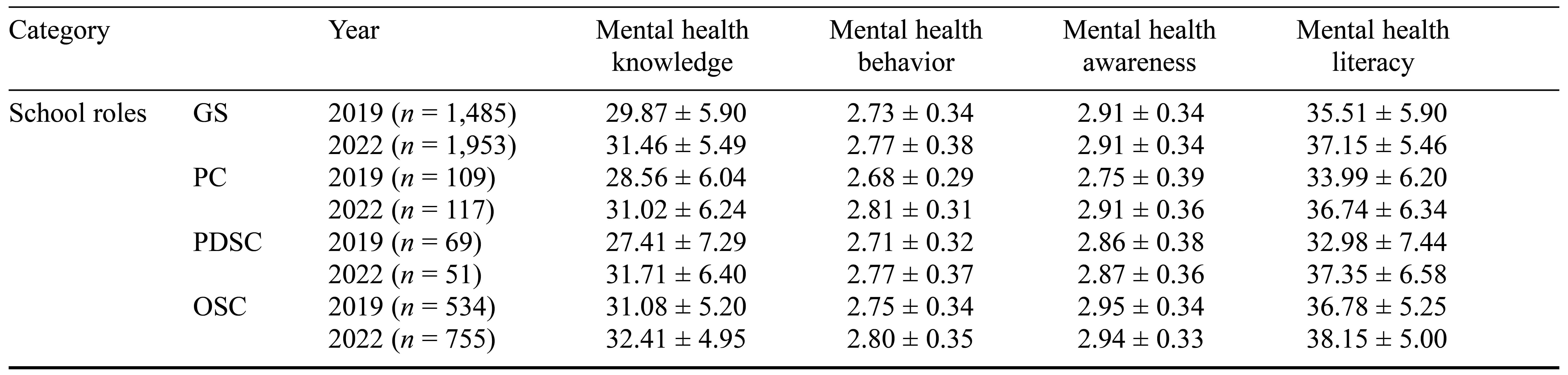
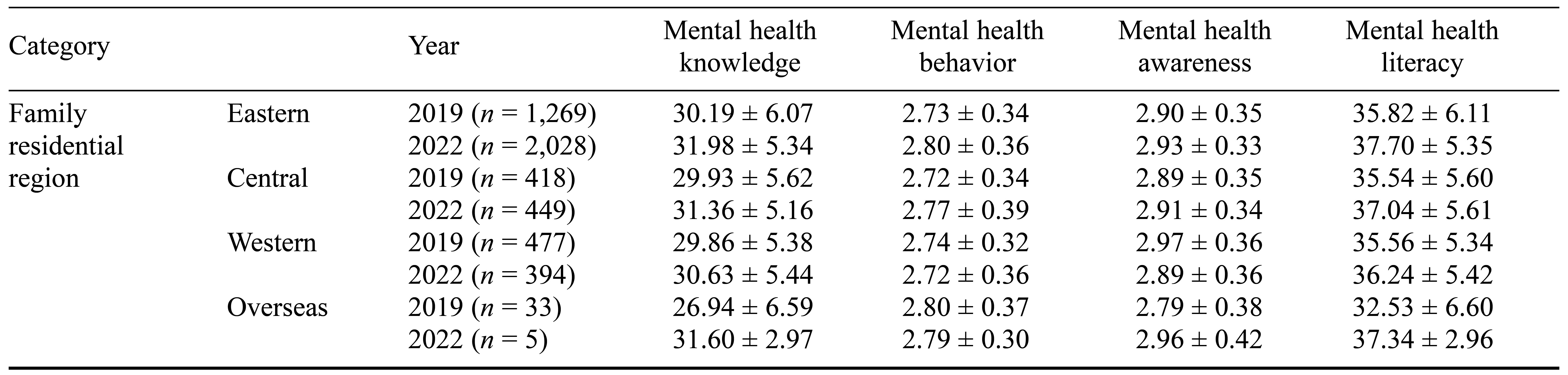
Analysis of Different Effects of School Roles on Mental Health Literacy Among College Students Before and During the COVID-19 Pandemic
To explore the difference in mental health literacy of college students according to their school roles before and during the COVID-19 pandemic, we conducted a two-way ANOVA of the interaction term of school roles (general students, psychological commissars, psychological department student cadres, other student cadres) and time period (prepandemic, during pandemic). The interaction term of school roles and time period had a significant effect on mental health knowledge, F(1, 3) = 2.96, p = .031, mental health awareness, F(1, 3) = 4.16, p = .006, and mental health literacy, F(1, 3) = 3.28, p = .020.
A simple effects analysis showed that general students, t = −8.32, p < .001, psychological commissars, t = 3.31, p = .021, psychological department student cadres, t = 4.18, p < .001, and other student cadres, t = 4.23, p < .001, scored higher on mental health knowledge during the pandemic compared with before the pandemic. In addition, general students, t = −8.53, p < .001, psychological commissars, t = 3.70, p = .005, psychological department student cadres, t = 4.23, p < .001, and other student cadres, t = 4.34, p < .001, scored higher on mental health literacy during the pandemic compared with before the pandemic. Among the four roles of college students, the psychological commissars scored higher on mental health awareness, t = 3.15, p = .011, during the COVID-19 pandemic compared with before the pandemic (see Table 4). The mental health knowledge and mental health literacy scores of all four groups were higher during the pandemic compared to before the pandemic. In addition, the mental health awareness scores of the psychological commissars were higher during the pandemic compared to beforehand.
Table 4. Comparison of the Impact of School Factors on College Students’ Mental Health Literacy Before and During the COVID-19 Pandemic
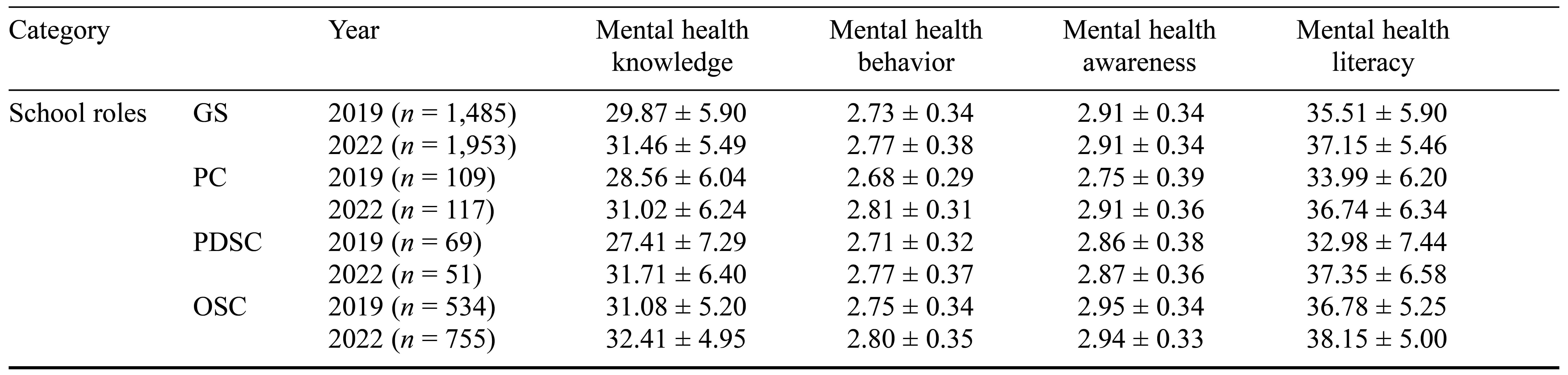
Note. Scores are mean ± standard deviation. GS = general students; PC = psychological commissars; PDSC = psychological department student cadres; OSC = other student cadres.
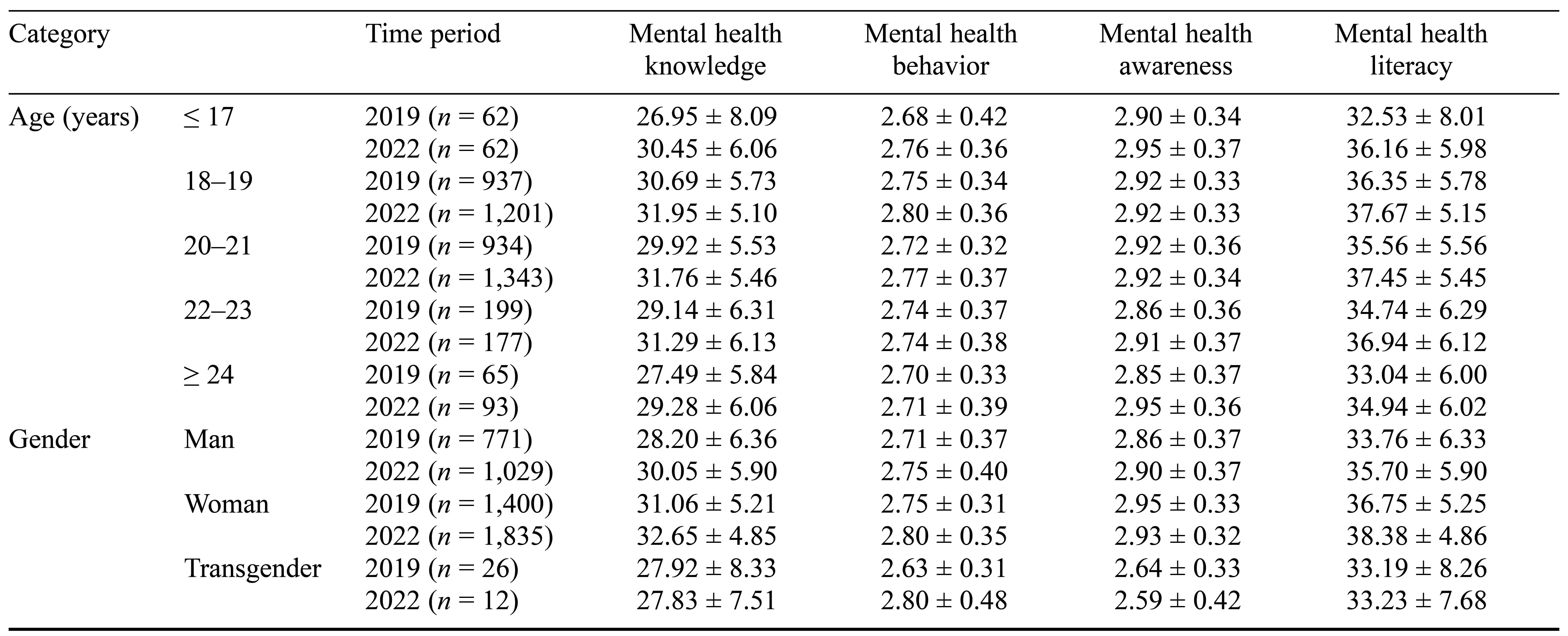
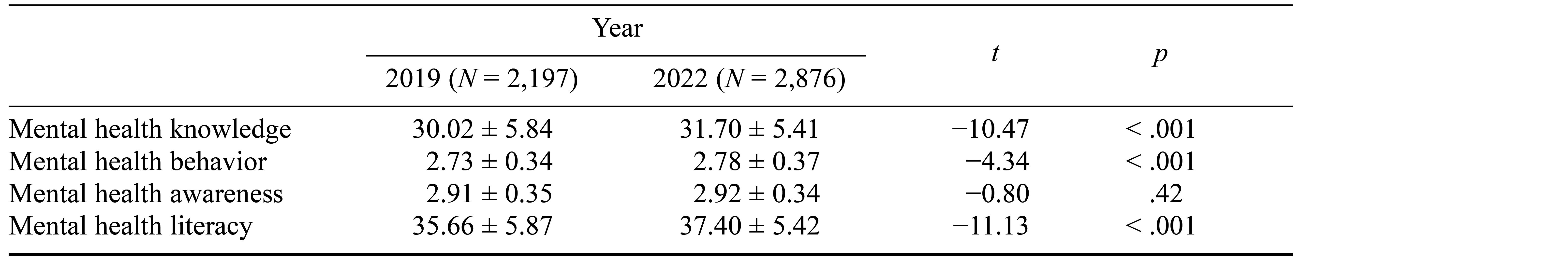
Analysis of Differences in Mental Health Literacy Among College Students According to Family Residential Regions Before and During the COVID-19 Pandemic
To explore the different effects of family residential region on the mental health literacy of college students before and during the COVID-19 pandemic, we conducted a two-way ANOVA of the interaction term of family residential region (eastern, central, western, overseas) and time period (2019, 2022). The interaction term of family residential region and time period had a significant effect on mental health behavior, F(1, 3) = 3.50, p = .005, mental health awareness, F(1, 3) = 5.41, p = .001, and mental health literacy, F(1, 3) = 3.11, p = .025. A simple effects analysis showed that mental health behavior was higher during the COVID-19 pandemic compared to before the pandemic among college students from the eastern region, t = 5.18, p < .001. College students in the western region scored lower on mental health awareness during the COVID-19 pandemic compared with beforehand, t = –3.23, p = .027, while college students in the eastern region, t = 9.38, p < .001, and central region, t = 3.94, p = .002, scored higher on mental health literacy during the COVID-19 pandemic compared with beforehand (see Table 5). These results suggest that college students in the eastern region showed positive changes in mental health behavior and mental health literacy, college students in the central region showed positive changes in mental health literacy, and college students in the western region showed negative changes.
Table 5. Comparison of the Impact of Family and Social Factors on College Students’ Mental Health Literacy Before and During the COVID-19 Pandemic
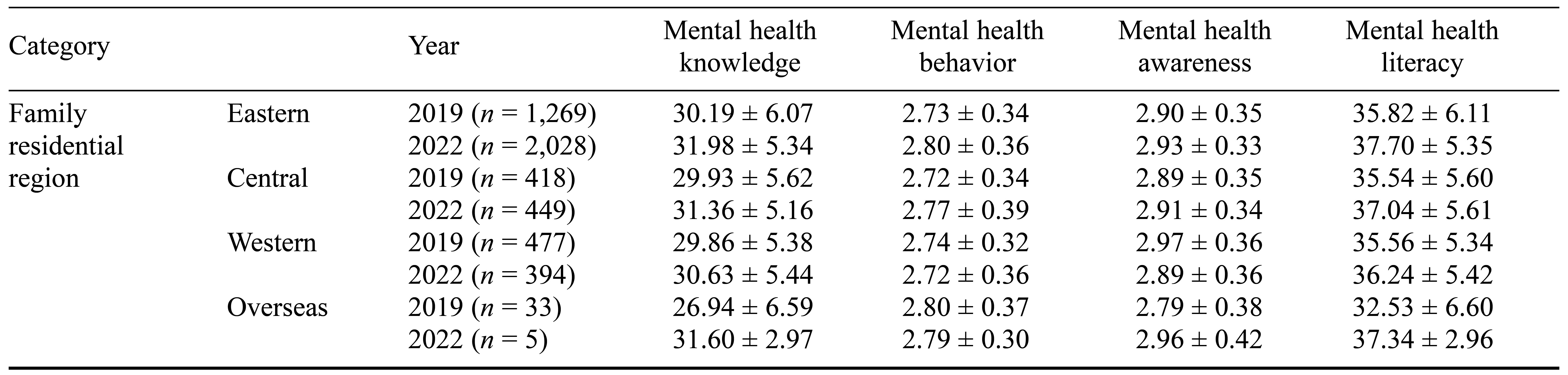
Note. Scores are mean ± standard deviation.
Discussion
Impact of the COVID-19 Pandemic on Mental Health Literacy
This study investigated whether there was a positive or negative impact of the COVID-19 pandemic on the mental health literacy of college students, with the goal of providing a foundation and recommendations for effective mental health education. The results show there were significant improvements in the mental health literacy (mental health knowledge, mental health behavior, mental health literacy) of college students during the COVID-19 pandemic compared with beforehand, which is in line with previous research findings indicating heightened awareness of mental health issues during times of crisis or significant societal changes (Aknin et al., 2022; Liu et al., 2020; Xiong et al., 2020; Zięba et al., 2022). The COVID-19 pandemic, characterized by widespread social isolation, economic uncertainty, and increased mental health challenges, likely prompted greater attention to mental health education and resources among college students (González-Sanguino et al., 2020). In addition, the widespread availability of mental-health-related activities, online resources, and virtual support services during the pandemic may have contributed to the observed improvements in mental health literacy (Pfefferbaum & North, 2020).
Cluster Analysis of Mental Health Literacy Groups
The clustering of students into those with high, moderate, and low mental health literacy aligns with findings from previous studies examining mental health literacy profiles among college populations (Yusoff et al., 2013). The observed increase in the proportion of students with high and moderate literacy during the COVID-19 pandemic is consistent with the notion that crises can stimulate proactive responses and promote resilience (Yang et al., 2021). However, further research is needed to explore the long-term stability of these clusters and their association with mental health outcomes over time.
Individual Factors and Mental Health Literacy
Whereas we found limited interactions between individual factors (e.g., age and gender) and mental health literacy, previous research had found no significant association of mental health literacy with age (Reavley & Jorm, 2011). However, gender differences in mental health literacy have been documented, with women often demonstrating higher levels of awareness and help-seeking behaviors than men do (Kecojevic et al., 2020; Vuelvas-Olmos et al., 2023; Wang et al., 2013). The change we observed in men’s mental health awareness during the COVID-19 pandemic may be attributed to targeted interventions or heightened media coverage addressing men’s mental health needs (Seidler et al., 2016). This finding emphasizes the necessity for targeted interventions to address gender-specific disparities in mental health literacy.
School Roles and Mental Health Literacy
Our findings highlight the role of the school environment in influencing mental health literacy, as we observed significant improvements across different school roles during the COVID-19 pandemic. This is consistent with previous research indicating the crucial role of the organizational structure and resources available within a college as well as school-based interventions in promoting mental health awareness and facilitating support initiatives among college students (Burns & Rapee, 2021; Eisenberg et al., 2013). Our findings show the effectiveness of designated roles such as psychological commissars, which aligns with previous research that examined interventions involving peer-led mental health programs in educational settings (El-Den et al., 2020). Psychological commissars may have played a pivotal role in disseminating mental health information and fostering supportive environments within their respective institutions, contributing to enhanced literacy levels among students. These activities may have enhanced knowledge and awareness of mental health, facilitated the identification and intervention of mental health problems, reduced the incidence of mental health issues, and subsequently improved the mental health status of college students during the pandemic.
Family Residential Regions and Mental Health Literacy
Our results indicate there were variations in mental health literacy across different residential regions, highlighting the influence of sociocultural factors on students’ understanding of mental health. This is consistent with previous research showing regional disparities in mental health literacy and help-seeking behaviors (Owens, 2019; Yusoff et al., 2013). Cultural norms, social support networks, and access to mental health services vary across regions, which can impact individuals’ attitudes and beliefs about mental health (Gulliver et al., 2010). The observed positive changes in mental health literacy among students in eastern and central regions during the COVID-19 pandemic may be attributed to regional differences in resource allocation, community support systems, and responsiveness to mental health needs (Liang et al., 2020).
Limitations and Future Research Directions
This study has some limitations. First, we distributed online questionnaires both before and during the COVID-19 pandemic using convenience sampling and snowball sampling, resulting in an uneven distribution of sample characteristic variables and a sample size exceeding those of most similar studies during the same period. However, we surveyed two different groups of students; thus, there is a possibility that the higher scores observed in the second group were equally high in this cohort prior to the pandemic. Second, our investigation of factors such as family socioeconomic status and social support was limited. Future research could analyze these aspects more comprehensively. Last, our study results are based primarily on the specific demographic and environmental conditions of the sample used. Although the results provide valuable insights, they may not be applicable when generalized to other groups, such as students of different age groups or those from other countries or cultural backgrounds. These different groups may have varying characteristics and experiences, which could influence the applicability of our findings. Further studies need to be conducted in various settings to assess the applicability and relevance of our findings in different contexts.
Conclusion
This study explored how college students’ mental health literacy has adapted in the face of the challenges brought about by the COVID-19 pandemic. The results provide valuable insights into the dynamics of mental health literacy, illuminating the complex interplay of individual, institutional, and sociocultural influences. These findings underscore the importance of tailored interventions and holistic approaches to mental health promotion in educational settings that take into account diverse student populations and contextual factors such as the economic and cultural characteristics of the family’s region.
References
Aknin, L. B., De Neve, J.-E., Dunn, E. W., Fancourt, D. E., Goldberg, E., Helliwell, J. F., ... Ben Amor, Y. (2022). Mental health during the first year of the COVID-19 pandemic: A review and recommendations for moving forward. Perspectives on Psychological Science, 17(4), 915–936.
Beasley, L., Kiser, R., & Hoffman, S. (2020). Mental health literacy, self-efficacy, and stigma among college students. Social Work in Mental Health, 18(6), 634–650.
Burns, J. R., & Rapee, R. M. (2021). From barriers to implementation: Advancing universal mental health screening in schools. Journal of Psychologists and Counsellors in Schools, 31(2), 172–183.
Cai, T., Zhuo, L., Chen, S., Miao, C., Wang, X., & Zhuo, L. (2021). Changes of health literacy among residents in a city before and after COVID-19 epidemic. Modern Preventive Medicine, 48(19), 3579–3582.
Eisenberg, D., Hunt, J., & Speer, N. (2013). Mental health in American colleges and universities: Variation across student subgroups and across campuses. The Journal of Nervous and Mental Disease, 201(1), 60–67.
El-Den, S., Moles, R., Choong, H.-J., & O’Reilly, C. (2020). Mental Health First Aid training and assessment among university students: A systematic review. Journal of the American Pharmacists Association, 60(5), e81–e95.
González-Sanguino, C., Ausín, B., Castellanos, M. Á., Saiz, J., López-Gómez, A., Ugidos, C., & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity, 87, 172–176.
Gulliver, A., Griffiths, K. M., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10(1), Article 113.
Healthy China Action. (2019–2030). 2019 Healthy China Action Promotion Committee [In Chinese].
Hu, Y., Ye, B., & Tan, J. (2021). Stress of COVID-19, anxiety, economic insecurity, and mental health literacy: A structural equation modeling approach. Frontiers in Psychology, 12, Article 707079.
Jorm, A. F. (2012). Mental health literacy: Empowering the community to take action for better mental health. The American Psychologist, 67(3), 231–243.
Jorm, A. F., Korten, A. E., Jacomb, P. A., Christensen, H., Rodgers, B., & Pollitt, P. (1997). “Mental health literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. The Medical Journal of Australia, 166(4), 182–186.
Kecojevic, A., Basch, C. H., Sullivan, M., & Davi, N. K. (2020). The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey: A cross-sectional study. PLoS ONE, 15(9), Article e0239696.
Liang, L., Ren, H., Cao, R., Hu, Y., Qin, Z., Li, C., & Mei, S. (2020). The effect of COVID-19 on youth mental health. The Psychiatric Quarterly, 91(3), 841–852.
Liu, S., Yang, L., Zhang, C., Xiang, Y.-T., Liu, Z., Hu, S., & Zhang, B. (2020). Online mental health services in China during the COVID-19 outbreak. The Lancet: Psychiatry, 7(4), e17–e18.
Ming, Z., & Chen, Z. (2020). Mental health literacy: Concept, measurement, intervention and effect [In Chinese]. Advancements in Psychological Science, 28(1), 1–12.
Owens, X. C. (2019). Mental health literacy among college students (Doctoral dissertation). University of Alaska Anchorage.
Pfefferbaum, B., & North, C. S. (2020). Mental health and the COVID-19 pandemic. The New England Journal of Medicine, 383(6), 510–512.
Reavley, N. J., & Jorm, A. F. (2011). National survey of mental health literacy and stigma. Canberra Department of Health and Ageing.
Reichel, J. L., Dietz, P., Sauter, C., Schneider, F., & Oenema, A. (2023). Is mental health literacy for depression associated with the intention toward preventive actions? A cross-sectional study among university students. Journal of American College Health, 71(5), 1530–1537.
Reis, A. C., Saheb, R., Moyo, T., Smith, C., & Sperandei, S. (2022). The impact of mental health literacy training programs on the mental health literacy of university students: A systematic review. Prevention Science, 23(4), 648–662.
Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41(1), 71–83.
Seidler, Z. E., Dawes, A. J., Rice, S. M., Oliffe, J. L., & Dhillon, H. M. (2016). The role of masculinity in men’s help-seeking for depression: A systematic review. Clinical Psychology Review, 49, 106–118.
Tambling, R. R., D’Aniello, C., & Russell, B. S. (2023). Mental health literacy: A critical target for narrowing racial disparities in behavioral health. International Journal of Mental Health and Addiction, 21, 1867–1881.
Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18.
Vuelvas-Olmos, C. R., Sánchez-Vidaña, D. I., & Cortés-Álvarez, N. Y. (2023). Gender-based analysis of the association between mental health, sleep quality, aggression, and physical activity among university students during the COVID-19 pandemic outbreak. Psychological Reports, 126(5), 2212–2236.
Wang, J., He, Y., Jiang, Q., Cai, J., Wang, W., Zeng, Q., ... Zhang, M. (2013). Mental health literacy among residents in Shanghai [In Chinese]. Shanghai Archives of Psychiatry, 25(4), 224–235.
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., ... McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64.
Yang, P., Ou, Y., Yang, H., Pei, X., Li, J., Wang, Y., ... Liu, W. (2021). Research on influencing factors and dimensions of health literacy in different age groups: Before and after the COVID-19 era in Chongqing, China. Frontiers in Public Health, 9, Article 690525.
Yusoff, M. S. B., Abdul Rahim, A. F., Baba, A. A., Ismail, S. B., Mat Pa, M. N., & Esa, A. R. (2013). Prevalence and associated factors of stress, anxiety and depression among prospective medical students. Asian Journal of Psychiatry, 6(2), 128–133.
Zięba, M., Wiecheć, K., Wójcik, N. E., & Zięba, M. J. (2022). Prioritizing positivity, styles of rumination, coping strategies, and posttraumatic growth: Examining their patterns and correlations in a prospective study. Frontiers in Psychology, 13, Article 842979.
Aknin, L. B., De Neve, J.-E., Dunn, E. W., Fancourt, D. E., Goldberg, E., Helliwell, J. F., ... Ben Amor, Y. (2022). Mental health during the first year of the COVID-19 pandemic: A review and recommendations for moving forward. Perspectives on Psychological Science, 17(4), 915–936.
Beasley, L., Kiser, R., & Hoffman, S. (2020). Mental health literacy, self-efficacy, and stigma among college students. Social Work in Mental Health, 18(6), 634–650.
Burns, J. R., & Rapee, R. M. (2021). From barriers to implementation: Advancing universal mental health screening in schools. Journal of Psychologists and Counsellors in Schools, 31(2), 172–183.
Cai, T., Zhuo, L., Chen, S., Miao, C., Wang, X., & Zhuo, L. (2021). Changes of health literacy among residents in a city before and after COVID-19 epidemic. Modern Preventive Medicine, 48(19), 3579–3582.
Eisenberg, D., Hunt, J., & Speer, N. (2013). Mental health in American colleges and universities: Variation across student subgroups and across campuses. The Journal of Nervous and Mental Disease, 201(1), 60–67.
El-Den, S., Moles, R., Choong, H.-J., & O’Reilly, C. (2020). Mental Health First Aid training and assessment among university students: A systematic review. Journal of the American Pharmacists Association, 60(5), e81–e95.
González-Sanguino, C., Ausín, B., Castellanos, M. Á., Saiz, J., López-Gómez, A., Ugidos, C., & Muñoz, M. (2020). Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain, Behavior, and Immunity, 87, 172–176.
Gulliver, A., Griffiths, K. M., & Christensen, H. (2010). Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry, 10(1), Article 113.
Healthy China Action. (2019–2030). 2019 Healthy China Action Promotion Committee [In Chinese].
Hu, Y., Ye, B., & Tan, J. (2021). Stress of COVID-19, anxiety, economic insecurity, and mental health literacy: A structural equation modeling approach. Frontiers in Psychology, 12, Article 707079.
Jorm, A. F. (2012). Mental health literacy: Empowering the community to take action for better mental health. The American Psychologist, 67(3), 231–243.
Jorm, A. F., Korten, A. E., Jacomb, P. A., Christensen, H., Rodgers, B., & Pollitt, P. (1997). “Mental health literacy”: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. The Medical Journal of Australia, 166(4), 182–186.
Kecojevic, A., Basch, C. H., Sullivan, M., & Davi, N. K. (2020). The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey: A cross-sectional study. PLoS ONE, 15(9), Article e0239696.
Liang, L., Ren, H., Cao, R., Hu, Y., Qin, Z., Li, C., & Mei, S. (2020). The effect of COVID-19 on youth mental health. The Psychiatric Quarterly, 91(3), 841–852.
Liu, S., Yang, L., Zhang, C., Xiang, Y.-T., Liu, Z., Hu, S., & Zhang, B. (2020). Online mental health services in China during the COVID-19 outbreak. The Lancet: Psychiatry, 7(4), e17–e18.
Ming, Z., & Chen, Z. (2020). Mental health literacy: Concept, measurement, intervention and effect [In Chinese]. Advancements in Psychological Science, 28(1), 1–12.
Owens, X. C. (2019). Mental health literacy among college students (Doctoral dissertation). University of Alaska Anchorage.
Pfefferbaum, B., & North, C. S. (2020). Mental health and the COVID-19 pandemic. The New England Journal of Medicine, 383(6), 510–512.
Reavley, N. J., & Jorm, A. F. (2011). National survey of mental health literacy and stigma. Canberra Department of Health and Ageing.
Reichel, J. L., Dietz, P., Sauter, C., Schneider, F., & Oenema, A. (2023). Is mental health literacy for depression associated with the intention toward preventive actions? A cross-sectional study among university students. Journal of American College Health, 71(5), 1530–1537.
Reis, A. C., Saheb, R., Moyo, T., Smith, C., & Sperandei, S. (2022). The impact of mental health literacy training programs on the mental health literacy of university students: A systematic review. Prevention Science, 23(4), 648–662.
Roberts, A. L., Gilman, S. E., Breslau, J., Breslau, N., & Koenen, K. C. (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41(1), 71–83.
Seidler, Z. E., Dawes, A. J., Rice, S. M., Oliffe, J. L., & Dhillon, H. M. (2016). The role of masculinity in men’s help-seeking for depression: A systematic review. Clinical Psychology Review, 49, 106–118.
Tambling, R. R., D’Aniello, C., & Russell, B. S. (2023). Mental health literacy: A critical target for narrowing racial disparities in behavioral health. International Journal of Mental Health and Addiction, 21, 1867–1881.
Tedeschi, R. G., & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15(1), 1–18.
Vuelvas-Olmos, C. R., Sánchez-Vidaña, D. I., & Cortés-Álvarez, N. Y. (2023). Gender-based analysis of the association between mental health, sleep quality, aggression, and physical activity among university students during the COVID-19 pandemic outbreak. Psychological Reports, 126(5), 2212–2236.
Wang, J., He, Y., Jiang, Q., Cai, J., Wang, W., Zeng, Q., ... Zhang, M. (2013). Mental health literacy among residents in Shanghai [In Chinese]. Shanghai Archives of Psychiatry, 25(4), 224–235.
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., ... McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64.
Yang, P., Ou, Y., Yang, H., Pei, X., Li, J., Wang, Y., ... Liu, W. (2021). Research on influencing factors and dimensions of health literacy in different age groups: Before and after the COVID-19 era in Chongqing, China. Frontiers in Public Health, 9, Article 690525.
Yusoff, M. S. B., Abdul Rahim, A. F., Baba, A. A., Ismail, S. B., Mat Pa, M. N., & Esa, A. R. (2013). Prevalence and associated factors of stress, anxiety and depression among prospective medical students. Asian Journal of Psychiatry, 6(2), 128–133.
Zięba, M., Wiecheć, K., Wójcik, N. E., & Zięba, M. J. (2022). Prioritizing positivity, styles of rumination, coping strategies, and posttraumatic growth: Examining their patterns and correlations in a prospective study. Frontiers in Psychology, 13, Article 842979.