Mental health and personality implications among medical students during the outbreak of the COVID-19 pandemic
Main Article Content
Few studies have explored the correlations between personality traits and mental health during the outbreak period of the COVID-19 pandemic. Thus, we conducted a cross-sectional survey to assess the personality traits and mental health of 142 students at Wenzhou Medical University, using the Generalized Anxiety Disorder 7-Item Scale, the Patient Health Questionnaire-9, the Sleep Status Self-Rating Scale, and the NEO Five-Factor Inventory. The results indicate that 30.28% of the sample had symptoms of anxiety, 40.85% had symptoms of depression, and 13.38% had disordered sleep. Neuroticism was positively correlated with anxiety, depression, and disordered sleep; extraversion was negatively correlated with anxiety, depression, and disordered sleep; openness was negatively correlated with disordered sleep; and conscientiousness was negatively correlated with both depression and disordered sleep. The results demonstrate that personality traits were risk factors for psychological disorders among students during the COVID-19 outbreak. Our findings may help provide a guide for screening for those susceptible to psychological disorders.
Since the first reported case in December 2019, coronavirus disease 2019 (COVID-19) has infected people throughout China and in many other countries around the globe (Chan et al., 2020; Holshue et al., 2020; Shereen et al., 2020; Stoecklin et al., 2020). Because of the high infectivity and mortality rate of COVID-19, humans face both severe psychological and physiological threats from this disease (Chew et al., 2020; Zhou et al., 2020). Many studies have found that psychological disorders such as anxiety, depression, and insomnia have prevailed during the COVID-19 pandemic (Elmer et al., 2020; Fu et al., 2020; X. Liu et al., 2020). Gaining greater understanding of the mental health of the general population throughout this pandemic could help guide intervention measures for preventing susceptible individuals from developing psychological disorders.
Personality is the relatively stable pattern of behaviors, thoughts, and feelings that characterize individuals (Caspi et al., 2005; Funder, 2001). The most-used model to describe personality traits is the five-factor model (Big Five; McCrae & Costa, 1987), in which the personality is categorized into five dimensions: neuroticism (i.e., being emotionally unstable), extraversion (i.e., being energetic/active and sociable), openness (i.e., being openminded and creative), agreeableness (i.e., willingness to cooperate and having compassion) and conscientiousness (i.e., being responsible and organized; Widiger & Trull, 1997).
According to their personality traits, people often exhibit different psychological and physiological responses to threats or pressure (Bibbey et al., 2013; Ruini et al., 2003). For example, one study conducted with a large Iranian sample found that the neuroticism was positively correlated with stress, anxiety, and depression (Alizadeh et al., 2018). In addition, in a sample of medical students, it was shown that extraversion was negatively correlated with the level of salivary immunoglobulin A, a marker of the stress response (Afrisham et al., 2016).
Among the personality traits of the Big Five model, it has usually been found that neuroticism and extraversion have opposite relationships with stressful responses. Many researchers have shown that people with a high level of neuroticism or a low level of extraversion are prone to being negatively affected by stress (Evans et al., 2016; Schneider et al., 2012; Uliaszek et al., 2010). In consideration of the high infectivity and mortality rate of COVID-19, people would probably have been susceptible to psychological stress when COVID-19 broke out, especially individuals with a high level of neuroticism. Individuals with a high level of extraversion might be prone to seek social–emotional support to alleviate the stress of the COVID-19 pandemic. Thus, we speculated that neuroticism would be positively correlated with psychological disorders and, in contrast, extraversion would be negatively correlated with psychological disorders during the outbreak of COVID-19.
Indeed, there have been some studies that support our speculation. For example, in a study conducted in the United States, Nikčević et al. (2021) found that residents’ neuroticism was positively correlated with anxiety and depression, and extraversion was negatively correlated with anxiety and depression during the COVID-19 pandemic. Further, S. Liu et al. (2021) and Murphy and Moret-Tatay (2021) found that neuroticism was positively correlated with stress during the COVID-19 pandemic and that perceived threat mediated this effect. In addition, Prentice et al. (2020) found that extraversion was significantly related to positive emotion-focused coping.
However, there are also some studies in which the findings did not support our speculation. For example, in a study conducted in Canada, S. Liu et al. (2021) found that higher neuroticism and extraversion were associated with higher levels of stress during the COVID-19 pandemic. In addition, in a study conducted in Korea, Han et al. (2021) found no significant correlation between neuroticism and anxiety, and in their study in Japan, Qian and Yahara (2020) found no significant correlation between extraversion and psychological disorders (stress, anxiety, and depression). However, similar studies have not yet been conducted in China. Thus, our aim in this study was to replicate these findings in the Chinese context, and to expand the scope of the research by also examining sleep problems and other demographic factors correlated with anxiety, depression, and sleep disorder.
In our cross-sectional study we examined the correlation between personality traits and psychological disorders (anxiety, depression, and disordered sleep) in a group of Chinese students during the outbreak of the COVID-19 pandemic. Here, we focused on the two personality traits of the Big Five model that are generally considered most relevant to stressful responses: neuroticism and extraversion (Hayes & Joseph, 2003), and formed the following hypotheses:
Hypothesis 1: Neuroticism will be positively correlated with psychological disorders.
Hypothesis 2: Extraversion will be negatively correlated with psychological disorders.
Method
Participants
This was a cross-sectional study conducted among students in Grades One to Four at Wenzhou Medical University (a detailed description of the sample is shown in Table 1). The exclusion criteria were as follows: (a) having suffered from a mental disorder before the COVID-19 pandemic, (b) currently taking medication for a mental disorder, and (c) not fully filling out the survey or submitted a survey with logical errors. Overall, 142 students submitted valid forms.
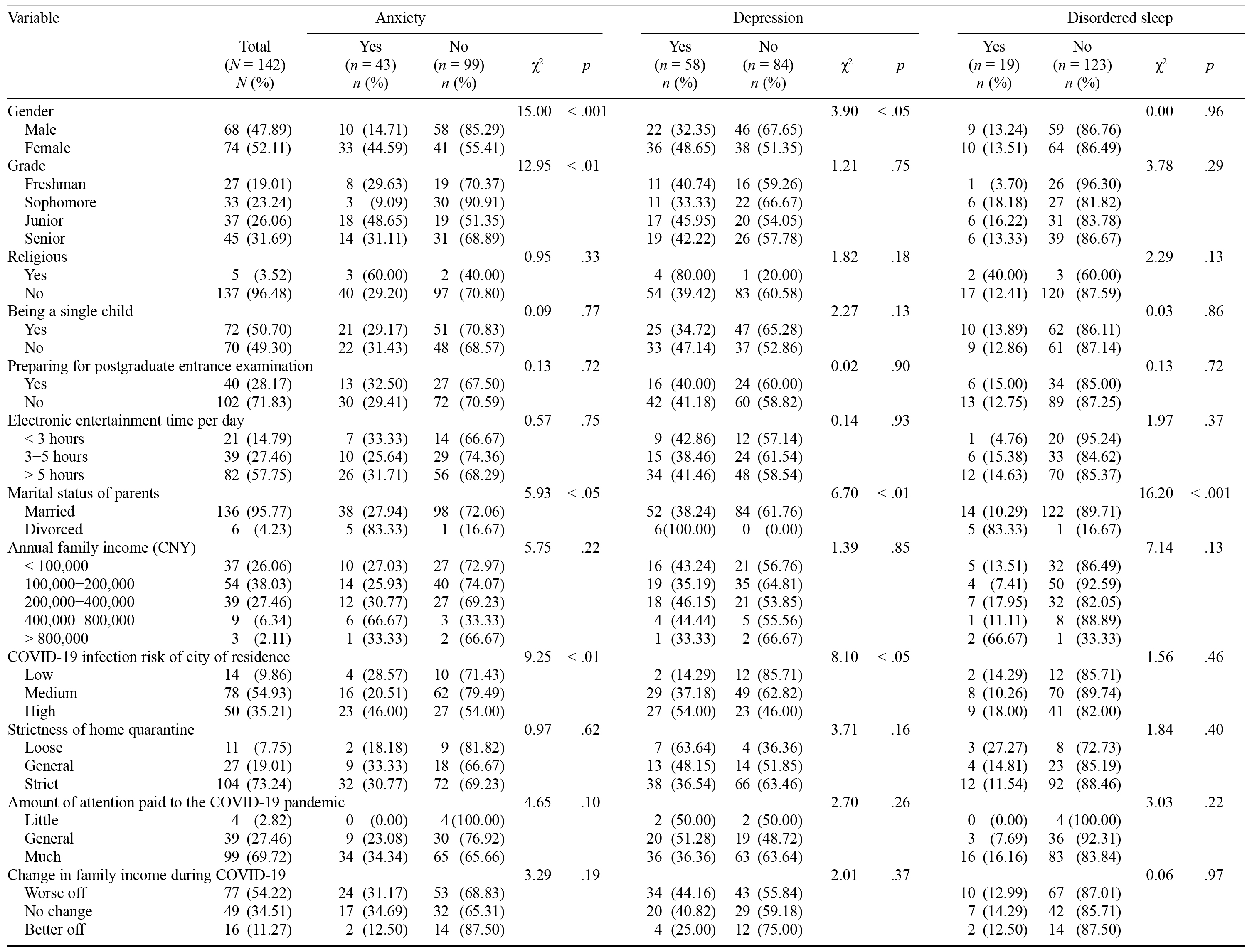
Table 1. Mental Health of the Respondents During the Outbreak of the COVID-19 Pandemic in China
Procedure
The study was conducted in March 2020. Students were asked to think about their mental health during the last month and respond to a series of measures were administered in the following order:
Demographic Questionnaire
Respondents provided (a) their grade, gender, religious orientation, postgraduate entrance examination preparation status, and daily hours spent using electronic entertainment products; (b) the marital status of their parents and their family’s income; (c) the COVID-19 infection risk in their place of residence and home quarantine strictness (see Table 1). We assumed that individuals spending more time playing electronic products would be less likely to develop psychological disorders during the COVID-19 pandemic outbreak.
Generalized Anxiety Disorder 7-Item Scale (GAD-7)
The GAD-7 is designed to assess anxiety symptoms (Spitzer et al., 2006). This scale comprises seven items (e.g., “I have trouble relaxing”) rated on a 4-point Likert scale ranging from 0 = not at all to 3 = nearly every day. The total GAD-7 score is categorized as follows: ≤ 4 indicates no anxiety, 5–9 indicates mild anxiety, 10–14 indicates moderate anxiety, and 15–21 indicates severe anxiety. We considered a total score of less than 5 to indicate the absence of anxiety and a total score of 5 or more to indicate the presence of anxiety. The GAD-7 scale has established validity and reliability, and Cronbach’s alpha coefficient was .88 in this study.
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 is designed to assess depression symptoms (Kroenke et al., 2001). This scale has nine items (e.g., “I have little interest or pleasure in doing things”) rated on a 4-point Likert scale ranging from 0 = not at all to 3 = nearly every day. The total PHQ-9 score is categorized as follows: ≤ 4 indicates no depression, 5–9 indicates mild depression, 10–14 indicates moderate depression, 15–19 indicates severe depression, and 20–27 indicates extremely severe depression. We regarded a total score of less than 5 to indicate the absence of depression and a total score of 5 or more to indicate the presence of depression. The PHQ-9 scale has established validity and reliability, and Cronbach’s alpha coefficient was .87 in this study.
Sleep Status Self-Rating Scale (SRSS)
The SRSS is used to evaluate sleep disorders (J. M. Li et al., 2000). This scale has 10 items (e.g., “I have difficulty falling asleep”) rated on a 5-point Likert scale from 1 = not at all to 5 = nearly every day. The higher the score, the poorer the sleep quality. The total SRSS score ranges from 10 (basically no sleep problems) to 50 (the most serious sleep problems). We regarded a total score < 23 to indicate no disordered sleep and a total score ≥ 23 to indicate poor-quality, disordered sleep. We selected the cutoff point of 23 in the SRSS according to a reference study by J. M. Li et al. (2000), in which the cutoff point for Chinese people with no disordered sleep was 22.14 ± 5.48. The SRSS scale has established validity and reliability, and Cronbach’s alpha coefficient was .88 in this study.
Neuroticism Extraversion Openness Five-Factor Inventory (NEO-FFI)
The NEO-FFI consists of 60 items designed to assess personality traits (Costa & McCrae, 1992). This scale includes five 12-item subscales: neuroticism, extraversion, openness, agreeableness, and conscientiousness. Sample items are as follows: “Sometimes I feel completely worthless” (neuroticism), “I laugh easily” (extraversion), “I often try new and foreign foods” (openness), “I try to be courteous to everyone I meet” (agreeableness), and “I keep my belongings neat and clean” (conscientiousness). Items are rated on a 5-point Likert scale ranging from 1 = strongly disagree to 5 = strongly agree. The NEO-FFI scale has established validity and reliability, and Cronbach’s alpha coefficients in this study were as follows: neuroticism = .82, extraversion = .82, openness = .67, agreeableness = .71, conscientiousness = .76.
Data Analysis
Data analysis was performed using SPSS software. Frequencies and percentages were used to describe the demographic variables. Chi-square tests were used to compare the differences in categorical variables. In addition, the variables were not normally distributed (Kolmogorov-Smirnov test: p < .05); thus, Spearman rank-order analysis was used to evaluate the correlations between the personality traits and anxiety, depression, or disordered sleep. The significance level for these analyses was set at .05. The probability values were Bonferroni corrected for multiple comparisons.
Results
Demographic Characteristics and Mental Health
We classified the city of residence of the respondents into three infection-risk levels according to the cumulative number of COVID-19 cases up until March 2020 (see Appendix). Detailed demographic information, including personal background, family background, and COVID-19-related information is presented in Table 1. Among the 142 respondents, 43 (30.28%) had symptoms of anxiety, 58 (40.85%) had symptoms of depression, and 19 (13.38%) had disordered sleep.
The Relationship Between Demographic Variables and Mental Health
The percentage of respondents with a psychological disorder differed significantly by gender, grade, marital status of parents, and COVID-19 infection risk of city of residence (see Table 1, χ2 test: p < .05). Women, compared to men, were more likely to suffer from anxiety (44.59% vs. 14.71%) and depression (48.65% vs. 32.35%). Juniors were more likely to suffer from anxiety (48.65%) compared to students in the other grades. Students whose parents were divorced showed greater anxiety (83.33%), more severe depression (100.00%), and more disordered sleep (83.33%) compared to those whose parents were married. Noticeably, a higher percentage of respondents living in a city with a high COVID-19 infection risk had symptoms of anxiety (46.00%) and depression (54.00%), compared with those living in a city with a lower infection risk.
The Relationship Between Personality Traits and Mental Health
As shown in Table 2, neuroticism was significantly and positively correlated with anxiety, depression, and disordered sleep; extraversion was significantly and negatively correlated with anxiety, depression, and disordered sleep; openness was significantly and negatively correlated with disordered sleep; and conscientiousness was significantly and negatively correlated with both depression and disordered sleep.
Table 2. Correlations Between Mental Health and Personality Traits
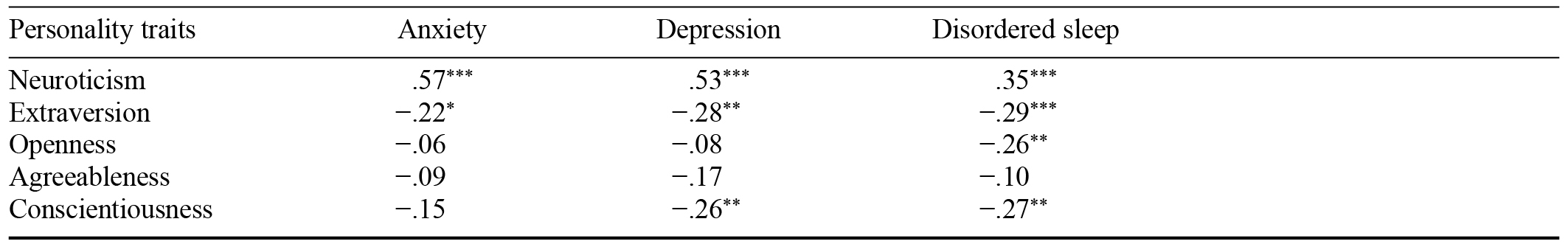
Note. Significance level was Bonferroni corrected.
* p < .05. ** p < .01. *** p < .001.
Discussion
In this cross-sectional study we assessed the mental health and personality traits of students at Wenzhou Medical University in March 2020, during the outbreak of the COVID-19 pandemic. The results demonstrate that a high percentage of these students had psychological disorders. The figures are higher than those reported in previous similar studies conducted with Chinese students during the COVID-19 pandemic in which it was consistently reported that around 12% had symptoms of anxiety, 9% had symptoms of depression, and 3% were experiencing poor sleep quality (X. Li et al., 2020; Sun et al., 2020; Tang et al., 2020). This discrepancy is possibly owing to differences in sample characteristics, methods for psychological assessment, or severity of the COVID-19 pandemic in the respondents’ respective cities of residence. However, in a recent review Xiong et al. (2020) reported that the prevalence of anxiety in the Chinese general population during the COVID-19 pandemic ranged from 6.33% to 50.9% and the prevalence of depression ranged from 14.6% to 48.3%. Generally, our findings are consistent with those of many previous studies demonstrating a negative correlation between the COVID-19 pandemic and the mental health of college students in China and other countries around the world (Dhar et al., 2020; Husky et al., 2020; Lyons et al., 2020; Marelli et al., 2020; Tang et al., 2020; Torun & Torun, 2020).
We found that gender, grade, marital status of parents, and COVID-19 infection risk of city of residence were risk factors for developing psychological disorders during the COVID-19 outbreak. These results are consistent with previous reports (Fu et al., 2020; X. Li et al., 2020; Wang et al., 2020; Zhu et al., 2020). These results imply that during the COVID-19 outbreak, the degree of threat of infection was the deciding factor in whether respondents experienced symptoms of psychological disorders. This speculation was supported by X. Li et al. (2020), who found that students’ perceptions of the level of risk of COVID-19 infection were correlated with how much psychological stress they experienced during the COVID-19 outbreak. However, we found that home quarantine was not a risk factor. This was probably because of the respondents’ perception of confinement measures during the COVID-19 outbreak as loose rather than strict (see Table 1). In comparison, some studies found that home quarantine was positively correlated with psychological disorders during the period of national lockdown (Elmer et al., 2020; Husky et al., 2020; Khan et al., 2020).
Notably, we found that personality traits were also risk factors for experiencing psychological disorders during the COVID-19 outbreak. This is consistent with the findings of previous studies in which personality traits were assessed with the Big Five model (Nikčević et al., 2021; Osimo et al., 2021) or the Dark Tetrad model (Hardin et al., 2021). Moreover, other studies have reported that personality traits are strongly correlated with psychological and behavioral responses to the COVID-19 pandemic, such as concern, emotion, and precaution measures (Aschwanden et al., 2020; de Francisco Carvalho et al., 2020; Garbe et al., 2020; Somma et al., 2020). These results highlight the importance of personality traits in mediating psychological responses during the COVID-19 pandemic. According to the framework proposed by Bolger and Zuckerman (1995), personality affects both exposure and reactivity to stressful events, which could explain how personality affected mental health during the COVID-19 pandemic.
Limitations and Directions for Future Research
There are several limitations to this study that should be noted: First, this was a cross-sectional study; thus, we cannot draw causal inferences. Second, students at Wenzhou Medical University were the only group in the survey. The limited and small sample size may not represent the full student population in China. Third, we conducted this study using only self-report measures, which may be affected by subjective error. Finally, the demographic characteristics we examined are not comprehensive, and there may be other factors that have a close correlation with mental health. Nonetheless, our findings provide a valuable understanding of the demographic characteristics and personality traits that correlate with the mental health of medical students during the COVID-19 outbreak.
Conclusion
The COVID-19 pandemic has imposed a significant psychological threat for people around the globe. Individuals may show different psychological responses to the COVID-19 threat according to their demographic characteristics or personality traits. In this study we found that several demographic variables were risk factors for anxiety, depression, and disordered sleep among Chinese medical students during the COVID-19 outbreak. In addition, personality traits were closely correlated with psychological disorders. These findings may provide a guide for the screening of populations susceptible to psychological disorders, and for the provision of targeted psychological interventions during the COVID-19 pandemic.
References
Afrisham, R., Sadegh-Nejadi, S., SoliemaniFar, O., Kooti, W., Ashtary-Larky, D., Alamiri, F., ... Khaneh-Keshi, A. (2016). Salivary testosterone levels under psychological stress and its relationship with rumination and five personality traits in medical students. Psychiatry Investigation, 13(6), 637–643.
https://doi.org/10.4306/pi.2016.13.6.637
Alizadeh, Z., Feizi, A., Rejali, M., Afshar, H., Keshteli, A. H., & Adibi, P. (2018). The predictive value of personality traits for psychological problems (stress, anxiety and depression): Results from a large population based study. Journal of Epidemiology and Global Health, 8(3–4), 124–133.
https://doi.org/10.2991/j.jegh.2017.11.003
Aschwanden, D., Strickhouser, J. E., Amanda, A. S., Lee, J. H., Luchetti, M., Stephan, Y., … Terracciano, A. (2020). Psychological and behavioural responses to coronavirus disease 2019: The role of personality. European Journal of Personality, 35(1), 51–66.
https://doi.org/10.1002/per.2281
Bibbey, A., Carroll, D., Roseboom, T. J., Phillips, A. C., & de Rooij, S. R. (2013). Personality and physiological reactions to acute psychological stress. International Journal of Psychophysiology, 90(1), 28–36.
https://doi.org/10.1016/j.ijpsycho.2012.10.018
Bolger, N., & Zuckerman, A. (1995). A framework for studying personality in the stress process. Journal of Personality and Social Psychology, 69(5), 890–902.
https://doi.org/10.1037/0022-3514.69.5.890
Caspi, A., Roberts, B. W., & Shiner, R. L. (2005). Personality development: Stability and change. Annual Review of Psychology, 56, 453–484.
https://doi.org/10.1146/annurev.psych.55.090902.141913
Chan, J. F.-W., Yuan, S., Kok, K.-H., To, K. K.-W., Chu, H., Yang, J., … Yuen, K.-Y. (2020). A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet, 395(10223), 514–523.
https://doi.org/10.1016/S0140-6736(20)30154-9
Chew, N. W. S., Lee, G. K. H., Tan, B. Y. Q., Jing, M., Goh, Y., Ngiam, N. J. H., … Sharma, V. K. (2020). A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity, 88, 559–565.
https://doi.org/10.1016/j.bbi.2020.04.049
Costa, P. T., & McCrae, R. R. (1992). Revised NEO personality inventory (NEO-PR-I) and the five-factor inventory (NEO FFI): Professional manual. Psychological Assessment Resources.
de Francisco Carvalho, L., Pianowski, G., & Gonçalves, A. P. (2020). Personality differences and COVID-19: Are extroversion and conscientiousness personality traits associated with engagement with containment measures? Trends in Psychiatry and Psychotherapy, 42(2), 179–184.
http://doi.org/10.1590/2237-6089-2020-0029
Dhar, B. K., Ayittey, F. K., & Sarkar, S. M. (2020). Impact of COVID-19 on psychology among the university students. Global Challenges, 4(11), Article 2000038.
https://doi.org/10.1002/gch2.202000038
Elmer, T., Mepham, K., & Stadtfeld, C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One, 15(7), Article e0236337.
https://doi.org/10.1371/journal.pone.0236337
Evans, B. E., Stam, J., Huizink, A. C., Willemen, A. M., Westenberg, P. M., Branje, S., … van Lier, P. A. C. (2016). Neuroticism and extraversion in relation to physiological stress reactivity during adolescence. Biological Psychology, 117, 67–79.
https://doi.org/10.1016/j.biopsycho.2016.03.002
Fu, W., Wang, C., Zou, L., Guo, Y., Lu, Z., Yan, S., & Mao, J. (2020). Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Translational Psychiatry, 10(1), Article 225.
https://doi.org/10.1038/s41398-020-00913-3
Funder, D. C. (2001). Personality. Annual Review of Psychology, 52, 197–221.
https://doi.org/10.1146/annurev.psych.52.1.197
Garbe, L., Rau, R., & Toppe, T. (2020). Influence of perceived threat of COVID-19 and HEXACO personality traits on toilet paper stockpiling. PLoS ONE, 15(6), Article e0234232.
https://doi.org/10.1371/journal.pone.0234232
Han, Y., Jang, J., Cho, E., & Choi, K.-H. (2021). Investigating how individual differences influence responses to the COVID-19 crisis: The role of maladaptive and five-factor personality traits. Personality and Individual Differences, 176, Article 110786.
https://doi.org/10.1016/j.paid.2021.110786
Hardin, B. S., Smith, C. V., & Jordan, L. N. (2021). Is the COVID-19 pandemic even darker for some? Examining dark personality and affective, cognitive, and behavioral responses to the COVID-19 pandemic. Personality and Individual Differences, 171, Article 110504.
https://doi.org/10.1016/j.paid.2020.110504
Hayes, N., & Joseph, S. (2003). Big 5 correlates of three measures of subjective wellbeing. Personality and Individual Differences, 34(4), 723–727.
https://doi.org/10.1016/S0191-8869(02)00057-0
Holshue, M. L., DeBolt, C., Lindquist, S., Lofy, K. H., Wiesman, J., Bruce, H., … Cohn, A. (2020). First case of 2019 novel coronavirus in the United States. The New England Journal of Medicine, 382(10), 929–936.
https://doi.org/10.1056/NEJMoa2001191
Husky, M. M., Kovess-Masfety, V., & Swendsen, J. D. (2020). Stress and anxiety among university students in France during COVID-19 mandatory confinement. Comprehensive Psychiatry, 102, Article 152191.
https://doi.org/10.1016/j.comppsych.2020.152191
Khan, A. H., Sultana, M. S., Hossain, S., Hasan, M. T., Ahmed, H. U., & Sikder, M. T. (2020). The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. Journal of Affective Disorders, 277, 121–128.
https://doi.org/10.1016/j.jad.2020.07.135
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613.
https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Li, J. M., Yin, S. F., Duan, J. X., & Zhang, Q. B. (2000). Analysis rating of sleep state of 13,273 normal persons [In Chinese]. Health Psychology Journal, 8(3), 351–354.
https://doi.org/10.3969/j.issn.1005-1252.2000.03.057
Li, X., Lv, S., Liu, L., Chen, R., Chen, J., Liang, S., … Zhao, J. (2020). COVID-19 in Guangdong: Immediate perceptions and psychological impact on 304,167 college students. Frontiers in Psychology, 11, Article 2024.
https://doi.org/10.3389/fpsyg.2020.02024
Liu, S., Lithopoulos, A., Zhang, C.-Q., Garcia-Barrera, M. A., & Rhodes, R. E. (2021). Personality and perceived stress during COVID-19 pandemic: Testing the mediating role of perceived threat and efficacy. Personality and Individual Differences, 168, Article 110351.
https://doi.org/10.1016/j.paid.2020.110351
Liu, X., Luo, W.-T., Li, Y., Li, C.-N., Hong, Z.-S., Chen, H.-L., … Xia, J.-Y. (2020). Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infectious Diseases of Poverty, 9(1), Article 58.
https://doi.org/10.1186/s40249-020-00678-3
Lyons, Z., Wilcox, H., Leung, L., & Dearsley, O. (2020). COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australasian Psychiatry, 28(6), 649–652.
https://doi.org/10.1177/1039856220947945
Marelli, S., Castelnuovo, A., Somma, A., Castronovo, V., Mombelli, S., Bottoni, D., … Ferini-Strambi, L. (2020). Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of Neurology, 268, 8–15.
https://doi.org/10.1007/s00415-020-10056-6
McCrae, R. R., & Costa, P. T. (1987). Validation of the five-factor model of personality across instruments and observers. Journal of Personality and Social Psychology, 52(1), 81–90.
https://doi.org/10.1037//0022-3514.52.1.81
Murphy, M., & Moret-Tatay, C. (2021). Personality and attitudes confronting death awareness during the COVID-19 outbreak in Italy and Spain. Frontiers in Psychiatry, 12, Article 627018.
https://doi.org/10.3389/fpsyt.2021.627018
Nikčević, A. V., Marino, C., Kolubinski, D. C., Leach, D., & Spada, M. M. (2021). Modelling the contribution of the Big Five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. Journal of Affective Disorders, 279, 578–584.
https://doi.org/10.1016/j.jad.2020.10.053
Osimo, S. A., Aiello, M., Gentili, C., Ionta, S., & Cecchetto, C. (2021). The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Frontiers in Psychology, 12, Article 630751.
https://doi.org/10.3389/fpsyg.2021.630751
Prentice, C., Zeidan, S., & Wang, X. (2020). Personality, trait EI and coping with COVID 19 measures. International Journal of Disaster Risk Reduction, 51, Article 101789.
https://doi.org/10.1016/j.ijdrr.2020.101789
Qian, K., & Yahara, T. (2020). Mentality and behavior in COVID-19 emergency status in Japan: Influence of personality, morality and ideology. PLoS One, 15(7), Article e0235883.
https://doi.org/10.1371/journal.pone.0235883
Ruini, C., Ottolini, F., Rafanelli, C., Tossani, E., Ryff, C. D., & Fava, G. A. (2003). The relationship of psychological well-being to distress and personality. Psychotherapy and Psychosomatics, 72(5), 268–275.
https://doi.org/10.1159/000071898
Schneider, T. R., Rench, T. A., Lyons, J. B., & Riffle, R. R. (2012). The influence of neuroticism, extraversion and openness on stress responses. Stress and Health, 28(2), 102–110.
https://doi.org/10.1002/smi.1409
Shereen, M. A., Khan, S., Kazmi, A., Bashir, N., & Siddique, R. (2020). COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research, 24, 91–98.
https://doi.org/10.1016/j.jare.2020.03.005
Somma, A., Gialdi, G., Krueger, R. F., Markon, K. E., Frau, C., Lovallo, S., & Fossati, A. (2020). Dysfunctional personality features, non-scientifically supported causal beliefs, and emotional problems during the first month of the COVID-19 pandemic in Italy. Personality and Individual Differences, 165, Article 110139.
https://doi.org/10.1016/j.paid.2020.110139
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
https://doi.org/10.1001/archinte.166.10.1092
Stoecklin, S. B., Rolland, P., Silue, Y., Mailles, A., Campese, C., Simondon, A., … Levy-Bruhl, D. (2020). First cases of coronavirus disease 2019 (COVID-19) in France: Surveillance, investigations and control measures, January 2020. Eurosurveillance, 25(6), 20–26.
https://doi.org/10.2807/1560-7917.ES.2020.25.6.2000094
Sun, Y., Wang, D., Han, Z., Gao, J., Zhu, S., & Zhang, H. (2020). Disease prevention knowledge, anxiety, and professional identity during COVID-19 pandemic in nursing students in Zhengzhou, China. Journal of Korean Academy of Nursing, 50(4), 533–540.
https://doi.org/10.4040/jkan.20125
Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., Xie, C., … Xu, J. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders, 274, 1–7.
https://doi.org/10.1016/j.jad.2020.05.009
Torun, F., & Torun, S. D. (2020). The psychological impact of the COVID-19 pandemic on medical students in Turkey. Pakistan Journal of Medical Sciences, 36(6), 1355–1359.
https://doi.org/10.12669/pjms.36.6.2985
Uliaszek, A. A., Zinbarg, R. E., Mineka, S., Craske, M. G., Sutton, J. M., Griffith, J. W., … Hammen, C. (2010). The role of neuroticism and extraversion in the stress–anxiety and stress–depression relationships. Anxiety, Stress & Coping, 23(4), 363–381.
https://doi.org/10.1080/10615800903377264
Wang, Z.-H., Yang, H.-L., Yang, Y.-Q., Liu, D., Li, Z.-H., Zhang, X.-R., … Mao, C. (2020). Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. Journal of Affective Disorders, 275, 188–193.
https://doi.org/10.1016/j.jad.2020.06.034
Widiger, T. A., & Trull, T. J. (1997). Assessment of the five-factor model of personality. Journal of Personality Assessment, 68(2), 228–250.
https://doi.org/10.1207/s15327752jpa6802_2
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., … McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64.
https://doi.org/10.1016/j.jad.2020.08.001
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., … Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. The Lancet, 395(10229), 1054–1062.
https://doi.org/10.1016/S0140-6736(20)30566-3
Zhu, Z., Liu, Q., Jiang, X., Manandhar, U., Luo, Z., Zheng, X., … Zhang, B. (2020). The psychological status of people affected by the COVID-19 outbreak in China. Journal of Psychiatric Research, 129, 1–7.
https://doi.org/10.1016/j.jpsychires.2020.05.026
Appendix: Classification of COVID-19 Infection Risk According to the Cumulative Number of Cases in Each City in March 2020
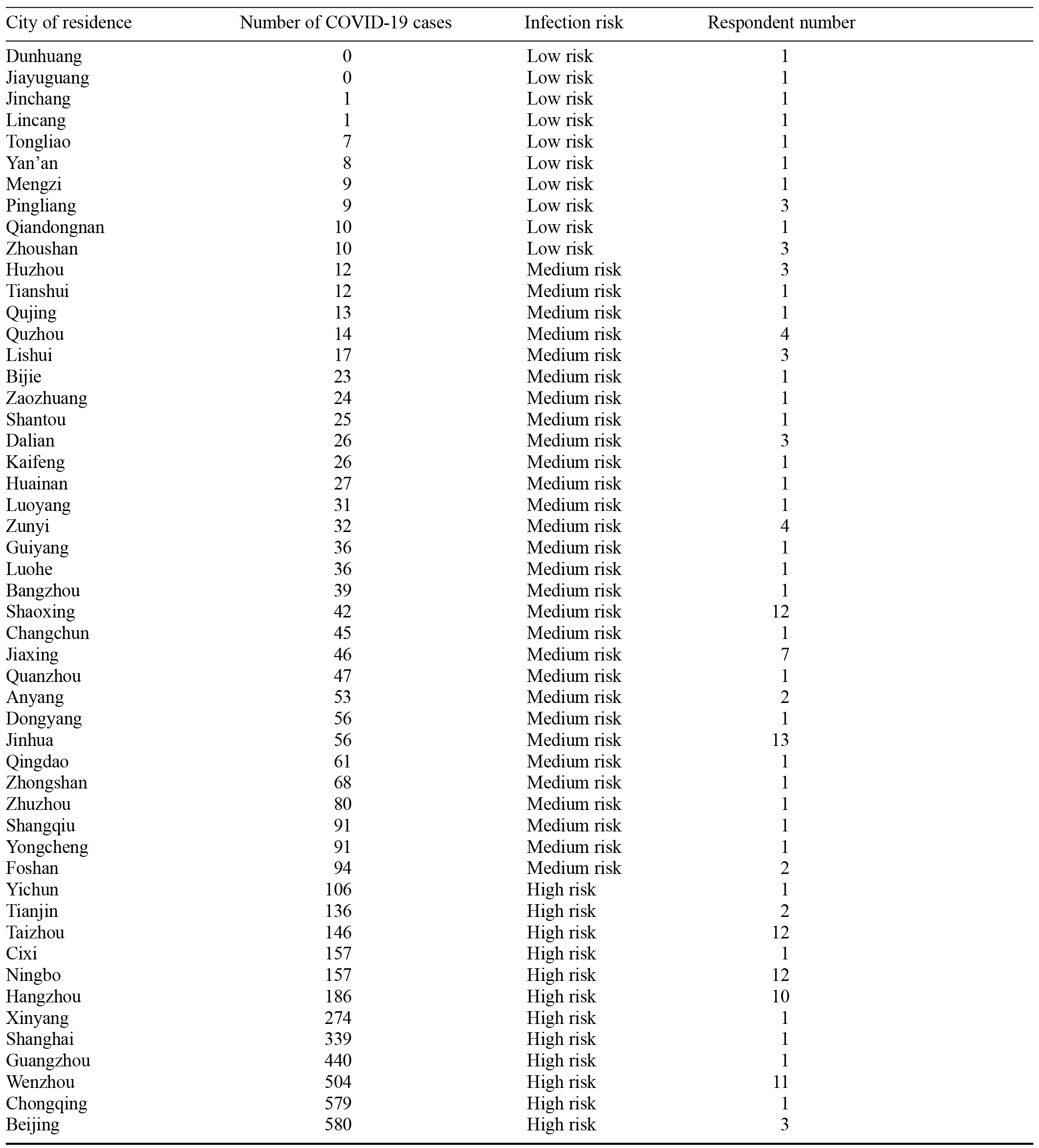
Note. Low risk = 0–10 cases; medium risk = 11–100 cases; high risk = over 100 cases.
Afrisham, R., Sadegh-Nejadi, S., SoliemaniFar, O., Kooti, W., Ashtary-Larky, D., Alamiri, F., ... Khaneh-Keshi, A. (2016). Salivary testosterone levels under psychological stress and its relationship with rumination and five personality traits in medical students. Psychiatry Investigation, 13(6), 637–643.
https://doi.org/10.4306/pi.2016.13.6.637
Alizadeh, Z., Feizi, A., Rejali, M., Afshar, H., Keshteli, A. H., & Adibi, P. (2018). The predictive value of personality traits for psychological problems (stress, anxiety and depression): Results from a large population based study. Journal of Epidemiology and Global Health, 8(3–4), 124–133.
https://doi.org/10.2991/j.jegh.2017.11.003
Aschwanden, D., Strickhouser, J. E., Amanda, A. S., Lee, J. H., Luchetti, M., Stephan, Y., … Terracciano, A. (2020). Psychological and behavioural responses to coronavirus disease 2019: The role of personality. European Journal of Personality, 35(1), 51–66.
https://doi.org/10.1002/per.2281
Bibbey, A., Carroll, D., Roseboom, T. J., Phillips, A. C., & de Rooij, S. R. (2013). Personality and physiological reactions to acute psychological stress. International Journal of Psychophysiology, 90(1), 28–36.
https://doi.org/10.1016/j.ijpsycho.2012.10.018
Bolger, N., & Zuckerman, A. (1995). A framework for studying personality in the stress process. Journal of Personality and Social Psychology, 69(5), 890–902.
https://doi.org/10.1037/0022-3514.69.5.890
Caspi, A., Roberts, B. W., & Shiner, R. L. (2005). Personality development: Stability and change. Annual Review of Psychology, 56, 453–484.
https://doi.org/10.1146/annurev.psych.55.090902.141913
Chan, J. F.-W., Yuan, S., Kok, K.-H., To, K. K.-W., Chu, H., Yang, J., … Yuen, K.-Y. (2020). A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet, 395(10223), 514–523.
https://doi.org/10.1016/S0140-6736(20)30154-9
Chew, N. W. S., Lee, G. K. H., Tan, B. Y. Q., Jing, M., Goh, Y., Ngiam, N. J. H., … Sharma, V. K. (2020). A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain, Behavior, and Immunity, 88, 559–565.
https://doi.org/10.1016/j.bbi.2020.04.049
Costa, P. T., & McCrae, R. R. (1992). Revised NEO personality inventory (NEO-PR-I) and the five-factor inventory (NEO FFI): Professional manual. Psychological Assessment Resources.
de Francisco Carvalho, L., Pianowski, G., & Gonçalves, A. P. (2020). Personality differences and COVID-19: Are extroversion and conscientiousness personality traits associated with engagement with containment measures? Trends in Psychiatry and Psychotherapy, 42(2), 179–184.
http://doi.org/10.1590/2237-6089-2020-0029
Dhar, B. K., Ayittey, F. K., & Sarkar, S. M. (2020). Impact of COVID-19 on psychology among the university students. Global Challenges, 4(11), Article 2000038.
https://doi.org/10.1002/gch2.202000038
Elmer, T., Mepham, K., & Stadtfeld, C. (2020). Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One, 15(7), Article e0236337.
https://doi.org/10.1371/journal.pone.0236337
Evans, B. E., Stam, J., Huizink, A. C., Willemen, A. M., Westenberg, P. M., Branje, S., … van Lier, P. A. C. (2016). Neuroticism and extraversion in relation to physiological stress reactivity during adolescence. Biological Psychology, 117, 67–79.
https://doi.org/10.1016/j.biopsycho.2016.03.002
Fu, W., Wang, C., Zou, L., Guo, Y., Lu, Z., Yan, S., & Mao, J. (2020). Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Translational Psychiatry, 10(1), Article 225.
https://doi.org/10.1038/s41398-020-00913-3
Funder, D. C. (2001). Personality. Annual Review of Psychology, 52, 197–221.
https://doi.org/10.1146/annurev.psych.52.1.197
Garbe, L., Rau, R., & Toppe, T. (2020). Influence of perceived threat of COVID-19 and HEXACO personality traits on toilet paper stockpiling. PLoS ONE, 15(6), Article e0234232.
https://doi.org/10.1371/journal.pone.0234232
Han, Y., Jang, J., Cho, E., & Choi, K.-H. (2021). Investigating how individual differences influence responses to the COVID-19 crisis: The role of maladaptive and five-factor personality traits. Personality and Individual Differences, 176, Article 110786.
https://doi.org/10.1016/j.paid.2021.110786
Hardin, B. S., Smith, C. V., & Jordan, L. N. (2021). Is the COVID-19 pandemic even darker for some? Examining dark personality and affective, cognitive, and behavioral responses to the COVID-19 pandemic. Personality and Individual Differences, 171, Article 110504.
https://doi.org/10.1016/j.paid.2020.110504
Hayes, N., & Joseph, S. (2003). Big 5 correlates of three measures of subjective wellbeing. Personality and Individual Differences, 34(4), 723–727.
https://doi.org/10.1016/S0191-8869(02)00057-0
Holshue, M. L., DeBolt, C., Lindquist, S., Lofy, K. H., Wiesman, J., Bruce, H., … Cohn, A. (2020). First case of 2019 novel coronavirus in the United States. The New England Journal of Medicine, 382(10), 929–936.
https://doi.org/10.1056/NEJMoa2001191
Husky, M. M., Kovess-Masfety, V., & Swendsen, J. D. (2020). Stress and anxiety among university students in France during COVID-19 mandatory confinement. Comprehensive Psychiatry, 102, Article 152191.
https://doi.org/10.1016/j.comppsych.2020.152191
Khan, A. H., Sultana, M. S., Hossain, S., Hasan, M. T., Ahmed, H. U., & Sikder, M. T. (2020). The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. Journal of Affective Disorders, 277, 121–128.
https://doi.org/10.1016/j.jad.2020.07.135
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613.
https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Li, J. M., Yin, S. F., Duan, J. X., & Zhang, Q. B. (2000). Analysis rating of sleep state of 13,273 normal persons [In Chinese]. Health Psychology Journal, 8(3), 351–354.
https://doi.org/10.3969/j.issn.1005-1252.2000.03.057
Li, X., Lv, S., Liu, L., Chen, R., Chen, J., Liang, S., … Zhao, J. (2020). COVID-19 in Guangdong: Immediate perceptions and psychological impact on 304,167 college students. Frontiers in Psychology, 11, Article 2024.
https://doi.org/10.3389/fpsyg.2020.02024
Liu, S., Lithopoulos, A., Zhang, C.-Q., Garcia-Barrera, M. A., & Rhodes, R. E. (2021). Personality and perceived stress during COVID-19 pandemic: Testing the mediating role of perceived threat and efficacy. Personality and Individual Differences, 168, Article 110351.
https://doi.org/10.1016/j.paid.2020.110351
Liu, X., Luo, W.-T., Li, Y., Li, C.-N., Hong, Z.-S., Chen, H.-L., … Xia, J.-Y. (2020). Psychological status and behavior changes of the public during the COVID-19 epidemic in China. Infectious Diseases of Poverty, 9(1), Article 58.
https://doi.org/10.1186/s40249-020-00678-3
Lyons, Z., Wilcox, H., Leung, L., & Dearsley, O. (2020). COVID-19 and the mental well-being of Australian medical students: Impact, concerns and coping strategies used. Australasian Psychiatry, 28(6), 649–652.
https://doi.org/10.1177/1039856220947945
Marelli, S., Castelnuovo, A., Somma, A., Castronovo, V., Mombelli, S., Bottoni, D., … Ferini-Strambi, L. (2020). Impact of COVID-19 lockdown on sleep quality in university students and administration staff. Journal of Neurology, 268, 8–15.
https://doi.org/10.1007/s00415-020-10056-6
McCrae, R. R., & Costa, P. T. (1987). Validation of the five-factor model of personality across instruments and observers. Journal of Personality and Social Psychology, 52(1), 81–90.
https://doi.org/10.1037//0022-3514.52.1.81
Murphy, M., & Moret-Tatay, C. (2021). Personality and attitudes confronting death awareness during the COVID-19 outbreak in Italy and Spain. Frontiers in Psychiatry, 12, Article 627018.
https://doi.org/10.3389/fpsyt.2021.627018
Nikčević, A. V., Marino, C., Kolubinski, D. C., Leach, D., & Spada, M. M. (2021). Modelling the contribution of the Big Five personality traits, health anxiety, and COVID-19 psychological distress to generalised anxiety and depressive symptoms during the COVID-19 pandemic. Journal of Affective Disorders, 279, 578–584.
https://doi.org/10.1016/j.jad.2020.10.053
Osimo, S. A., Aiello, M., Gentili, C., Ionta, S., & Cecchetto, C. (2021). The influence of personality, resilience, and alexithymia on mental health during COVID-19 pandemic. Frontiers in Psychology, 12, Article 630751.
https://doi.org/10.3389/fpsyg.2021.630751
Prentice, C., Zeidan, S., & Wang, X. (2020). Personality, trait EI and coping with COVID 19 measures. International Journal of Disaster Risk Reduction, 51, Article 101789.
https://doi.org/10.1016/j.ijdrr.2020.101789
Qian, K., & Yahara, T. (2020). Mentality and behavior in COVID-19 emergency status in Japan: Influence of personality, morality and ideology. PLoS One, 15(7), Article e0235883.
https://doi.org/10.1371/journal.pone.0235883
Ruini, C., Ottolini, F., Rafanelli, C., Tossani, E., Ryff, C. D., & Fava, G. A. (2003). The relationship of psychological well-being to distress and personality. Psychotherapy and Psychosomatics, 72(5), 268–275.
https://doi.org/10.1159/000071898
Schneider, T. R., Rench, T. A., Lyons, J. B., & Riffle, R. R. (2012). The influence of neuroticism, extraversion and openness on stress responses. Stress and Health, 28(2), 102–110.
https://doi.org/10.1002/smi.1409
Shereen, M. A., Khan, S., Kazmi, A., Bashir, N., & Siddique, R. (2020). COVID-19 infection: Origin, transmission, and characteristics of human coronaviruses. Journal of Advanced Research, 24, 91–98.
https://doi.org/10.1016/j.jare.2020.03.005
Somma, A., Gialdi, G., Krueger, R. F., Markon, K. E., Frau, C., Lovallo, S., & Fossati, A. (2020). Dysfunctional personality features, non-scientifically supported causal beliefs, and emotional problems during the first month of the COVID-19 pandemic in Italy. Personality and Individual Differences, 165, Article 110139.
https://doi.org/10.1016/j.paid.2020.110139
Spitzer, R. L., Kroenke, K., Williams, J. B. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097.
https://doi.org/10.1001/archinte.166.10.1092
Stoecklin, S. B., Rolland, P., Silue, Y., Mailles, A., Campese, C., Simondon, A., … Levy-Bruhl, D. (2020). First cases of coronavirus disease 2019 (COVID-19) in France: Surveillance, investigations and control measures, January 2020. Eurosurveillance, 25(6), 20–26.
https://doi.org/10.2807/1560-7917.ES.2020.25.6.2000094
Sun, Y., Wang, D., Han, Z., Gao, J., Zhu, S., & Zhang, H. (2020). Disease prevention knowledge, anxiety, and professional identity during COVID-19 pandemic in nursing students in Zhengzhou, China. Journal of Korean Academy of Nursing, 50(4), 533–540.
https://doi.org/10.4040/jkan.20125
Tang, W., Hu, T., Hu, B., Jin, C., Wang, G., Xie, C., … Xu, J. (2020). Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. Journal of Affective Disorders, 274, 1–7.
https://doi.org/10.1016/j.jad.2020.05.009
Torun, F., & Torun, S. D. (2020). The psychological impact of the COVID-19 pandemic on medical students in Turkey. Pakistan Journal of Medical Sciences, 36(6), 1355–1359.
https://doi.org/10.12669/pjms.36.6.2985
Uliaszek, A. A., Zinbarg, R. E., Mineka, S., Craske, M. G., Sutton, J. M., Griffith, J. W., … Hammen, C. (2010). The role of neuroticism and extraversion in the stress–anxiety and stress–depression relationships. Anxiety, Stress & Coping, 23(4), 363–381.
https://doi.org/10.1080/10615800903377264
Wang, Z.-H., Yang, H.-L., Yang, Y.-Q., Liu, D., Li, Z.-H., Zhang, X.-R., … Mao, C. (2020). Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: A large cross-sectional study. Journal of Affective Disorders, 275, 188–193.
https://doi.org/10.1016/j.jad.2020.06.034
Widiger, T. A., & Trull, T. J. (1997). Assessment of the five-factor model of personality. Journal of Personality Assessment, 68(2), 228–250.
https://doi.org/10.1207/s15327752jpa6802_2
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., … McIntyre, R. S. (2020). Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders, 277, 55–64.
https://doi.org/10.1016/j.jad.2020.08.001
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., … Cao, B. (2020). Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. The Lancet, 395(10229), 1054–1062.
https://doi.org/10.1016/S0140-6736(20)30566-3
Zhu, Z., Liu, Q., Jiang, X., Manandhar, U., Luo, Z., Zheng, X., … Zhang, B. (2020). The psychological status of people affected by the COVID-19 outbreak in China. Journal of Psychiatric Research, 129, 1–7.
https://doi.org/10.1016/j.jpsychires.2020.05.026
Table 1. Mental Health of the Respondents During the Outbreak of the COVID-19 Pandemic in China
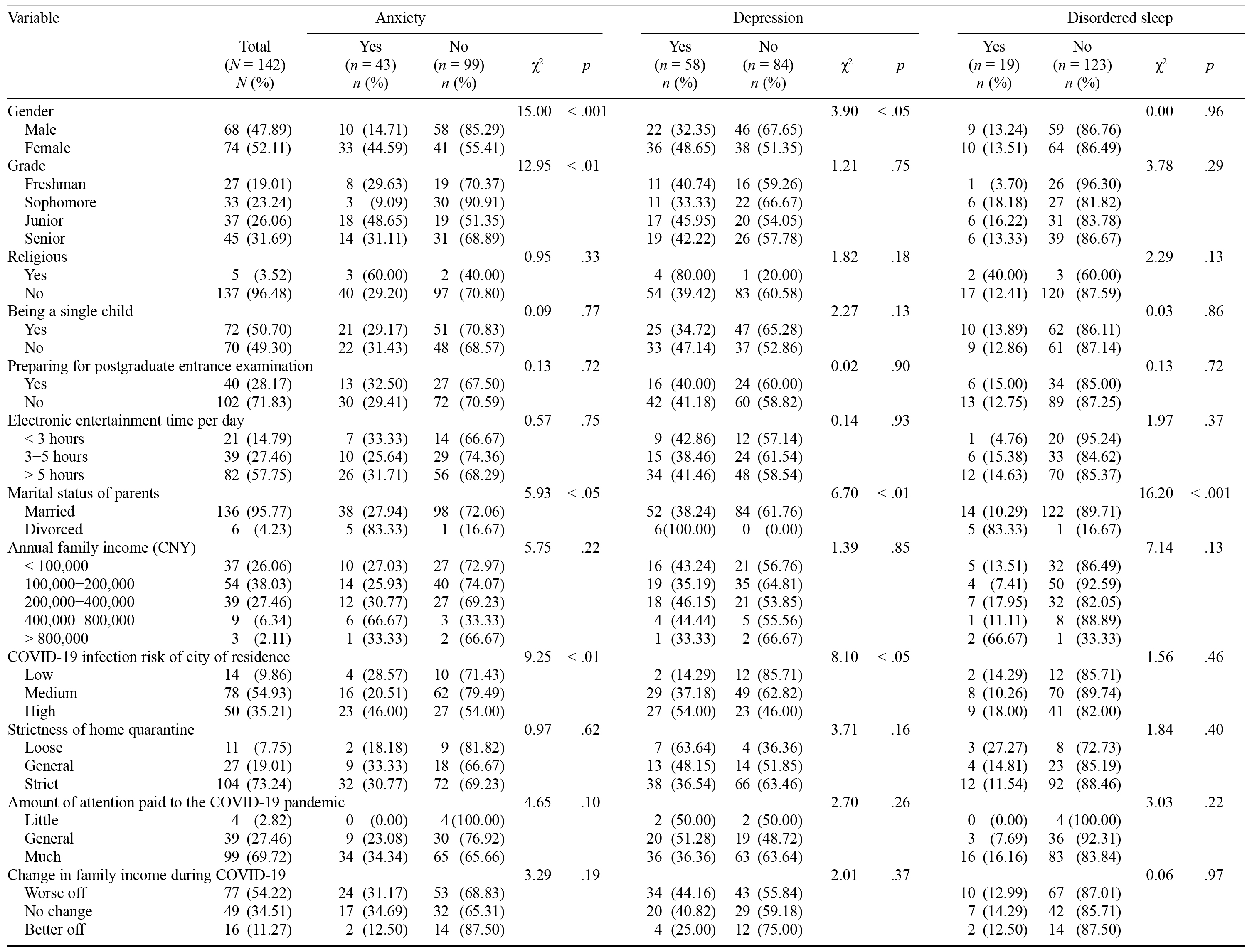
Table 2. Correlations Between Mental Health and Personality Traits
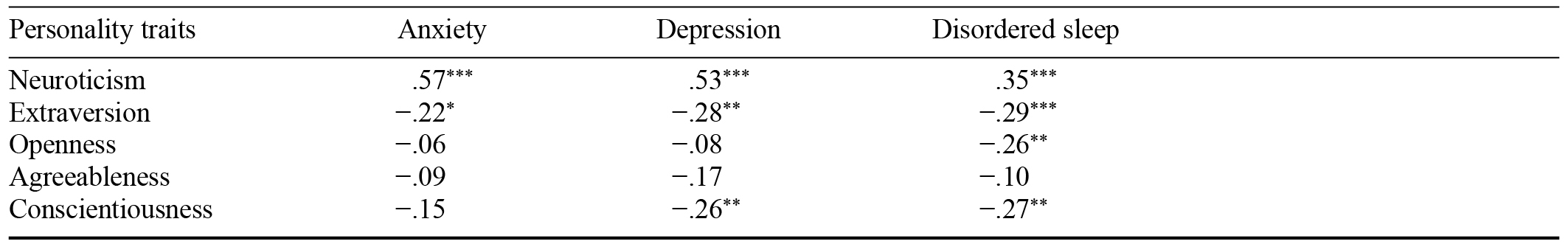
Note. Significance level was Bonferroni corrected.
* p < .05. ** p < .01. *** p < .001.
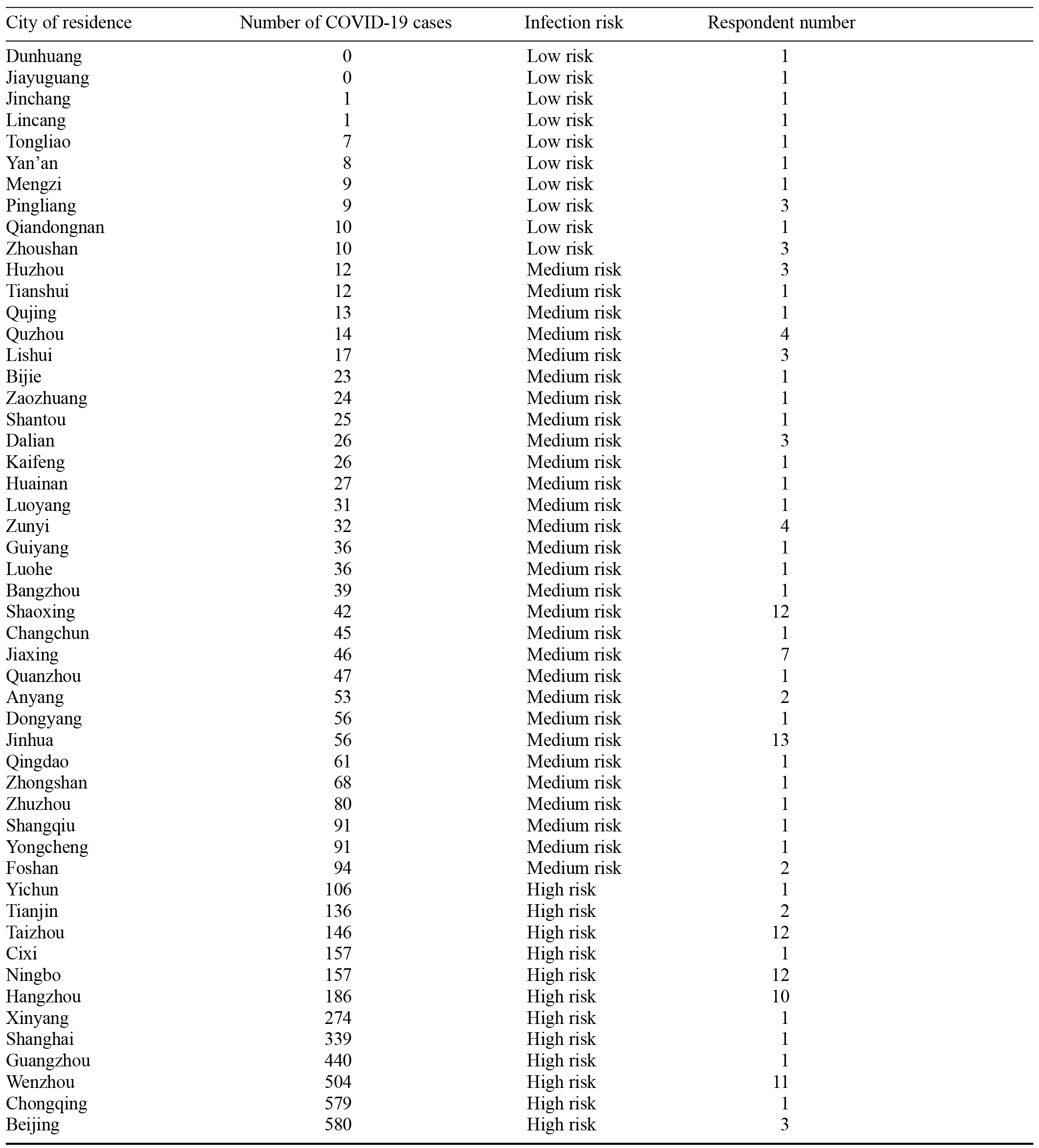
Note. Low risk = 0–10 cases; medium risk = 11–100 cases; high risk = over 100 cases.
This study was supported by grants from the research funds of Wenzhou Medical University (89219004 and wyx2020102005Z). The authors are thankful to the participants at Wenzhou Medical University.
Qi Wang, School of Mental Health, Wenzhou Medical University, Wenzhou, 325000, People’s Republic of China. Email: [email protected] or [email protected], or Changjin Li, School of Mental Health, Wenzhou Medical University, Wenzhou, 325000, People’s Republic of China. Email: [email protected]